December 24th, 2022 by Janine
The leaves I’m leaning over right now are the same colour as the vomit I’ve donated into the drain beside them. I laugh quietly, internally. Why am I thinking about leaves? Colours? Vomit? Why am I not even slightly anxious about the strangers watching me, possibly worrying about me, wondering if I’m ok or if they should or need to do anything to help me…or, in this post covid world, maybe they’re thinking about how to stay safe FROM me.

What do you think when you see someone unwell? Do you stay calm, slip into crisis management mode and think about helping? Do you get scared, wondering oh no, does she have it, have covid? Is she contagious? Is this some new horrible virus, the next pandemic? Both are normal reactions as is somewhere in between though the calm crisis management response is at least a little abnormal, a little wonderful, admirable and inspiring.
I’m not thinking about any of that, I’m noticing all the beautiful autumn colours of the leaves as they are squashed up against the sides of the drain and my chemo sickness slides down the grill over the top of them, beside them, disappearing into the deepest darkest London drain below. Wonder where it ends up? Does it pass under your house, my house? Or seep out into the underworld of this, vast, amazing city.

Gingerly, I unfold from my forward bend after what feels like half an hour. Only minutes have passed. I am relieved to see the open taxi door, the taxi driver’s patience as he waits for me to be ok enough to get back into the car. He hasn’t driven off; he doesn’t seem worried about me soiling his car, ruining his day. Thank goodness I splashed out on an exec car. I notice the slightly weird angle the car was holding in the street; the driver’s, unruffled (so grateful for that) rapid response (oh so very VERY grateful for that) as he had stopped the car when I had managed to whisper firmly stop now please, I’m going to be sick.

Shaky, trembling, feverish and nauseous, I did feel slightly better; certainly better than I had done all morning. I’d run late for a meeting, and then literally run to try and make it on time, only to find the person I was connecting with was sick too and had not bothered to tell his colleagues I was coming in. In the end, after breakfast on the house, getting something into my stomach to absorb the swathes of medication I’d downed and after a hopeful meeting with his apologetic colleague I felt safe again, listened to, cared about. I decided I had chosen the right venue for my upcoming shindig after all. The day wasn’t a complete disaster, in fact, so far most things had gone well.
Looking forward to being home and resting on the couch in front of the tv for the rest of the day, I crept back into the taxi, thanked the driver for his serenity and fluid driving skills, leant against the window and closed my eyes. I noticed how far I’d come, how I simply did not get embarrassed easily anymore, that feeling embarrassed, apologetic somehow, felt like a complete waste of my very precious time, energy and effort. I reminded myself embarrassment IS a valid feeling like all other feelings. Even though I wished we never had to experience embarrassment or shame. Those emotions crippled me in my early life and at various times throughout my teens, twenties and thirties. I had done anything to avoid embarrassment; the discomfort of being noticed in an unwanted way, of feeling shame, being caught out somehow, feeling the fool, of being judged naive, gullible or stupid.

Thank goodness I’m not so easily embarrassed anymore. I simply don’t care if I’m stared at while throwing up in the street, or when I do something wrong, make a mistake, am caught out, feel out of my depth or don’t know something. It’s easier than you think. Not caring doesn’t mean not taking responsibility; I still apologise when wrong, try to fix errors and am willing to quickly agree when I have misunderstood someone or something.
Yet remember, like me, you are human and just because you don’t know everything, or are sensitive and open enough to take something at face value and not realise someone is messing, teasing you, and above all you recognise you, me, we, ALL have, as much right, yes as much right as absolutely every other person…every other human being on this planet…to be here, to exist, to take up space, to have needs, wants, desires, have and use our voice.

We are as human enough as the next person therefore when I am being human, doing human things, like being unwell, throwing up, navigating chemotherapy, living life, craving being home on the couch…I don’t have to bother with embarrassment. I am already well and truly – ENOUGH.

New Treatment
I’m on a new treatment called DVD and it’s fairly heavy duty so no surprise I wasn’t going to get away unscathed. I want the regime to work. I need it to work if I am going to be able to hang about on this planet for a little longer; a little longer than the statistics still give me hope for. Anyway I’m here. I’m still here. I’m loving life, despite its challenges. I’m not going anywhere other than on travel adventures as much and as often as I can. I will be spending time with the most wonderful, special people I am privileged to have in my life, share this planet with as much and as often, as I can.
Happy holidays, Hanukkah and Christmas everyone regardless of what you do and don’t celebrate. I hope you are having an especially special break in whichever way suits YOU best.
Take care out there,
Janine
p.s. if anyone is hurting and needs support contact us at ComposurePsychology






Acknowledgements and References
Images: Me or courtesy of various artists on Unsplash.
© 2022 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Covid, Myeloma Treatment, Psychology for Cancer, Symptoms and Side Effects, Uncategorized Tagged with: Bortezomib (Velcade), Cancer, Chemotherapy, Daratumumab, Dexamethazone, DVD, emotions, Myeloma, Nausea, Psychology, RIchLife, Steroids, Treatment

July 25th, 2020 by Janine
Escape! I’m out of hospital. I burst into tears on leaving. Overwhelmed with a sense of freedom and loss. Loss of four weeks of my life and being in the world. Last night was my first night at home since June 27th. Twenty-six nights in one small poorly ventilated over heated room. Up until this experience I had never been in hospital for more than a few nights. Let’s hope I don’t end up back there which is common after a Stem Cell Transplant (SCT). Most people get an infection of some kind and have to go back in for a while. Afterall the immune system is still fairly non-existent. Though I think I’ve done my fair share of infection. E.Coli gripped me for at least two weeks of my four week stay. Not any old E.Coli either.
E.Coli
Specialist Nurse J came in yesterday. She asked me, do you know how sick you were? I said not really; I slept a lot and comparing my bad patch to awful gastro-enteritis which I have had a few times, in some ways it hadn’t seemed so bad. She set me straight, kindly.
She explained she had looked in on me a number of times but I had been asleep. This was a good thing because while most people have infection markers of 10 or below and doctors start getting worried and applying antibiotics, getting xrays, pet scans when infection markers are around 100, my infection marker registered over 400. My temp consistently spiked into 39s.
Nice. Once again I don’t do anything by halves. Trust me. I’m into full body experiences. Though thankfully I slept through a lot of this one! Instead of the Dr B predicted two week stay in hospital I was there 26 days and believe me once you feel well, hospital is not the place you want to be or at least definitely not cooped up in one room and one ward without being able to see the world.

Similar to e.coli
Relief
Two windows gave me moments of solace and a wee bit of interim escape. I could just see people playing basketball and tennis in Ruskin park through the tree canopy. Though the windows were in the sluice room which while spotless wasn’t a place I wanted to hang around much. Being reminded I may need to use a commode and other goodies at some stage in my hospital visit; if not now then next time wasn’t an image I needed in my mind. Being in there was handy one day; I grabbed a sick bowl for a moment of queasiness. Everything I needed right there, in the moment. Can’t ask for more than that.
The other HUGE thing that provided relief during this ordeal was all the fantastic facebook, insta, video, whatsapp messages I received. THANK YOU THANK YOU. Also for those I did manage to call for a few moments – thank you for being there, again and again. You are so so special, all of you.
SCT
The heavy duty chemo and return of my stem cells has appeared to go well and my neutrophils (basis of immune system) are on the rise. I did get mucositis (raw exposed soreness feeling in throat, mouth and oesophagus) which is common and I didn’t get it badly which I am thrilled about. My platelets are still a little low but heading in the right direction. Once I have hit the SCT + 100 day marker (October) I am due to have a bone marrow biopsy which is the deep breath moment. Will my bone marrow show any signs of Myeloma? Will it show a really low sign e.g. maybe a para protein (pp) of 1, similar or undetectable in my marrow? After all the cells that went back in were collected when my pp was 1. Or will it be higher? Will it come down? Questions, questions, patience needed. In the meantime I’m enjoying being home!
PICC Lines and Clots
PICC lines are good things and you can be unlucky with them. I’m a full not by halves person remember so with my first PICC line a clot arrived and ran up my arm above the PICC line towards my clavicle. If you saw the images on insta, you probably noticed my right arm and hand went an awful purple and swelled to about three times its size. After a week (I think I was a bit out of it) they took my PICC line out (nasty little buggers – they have a fish hook style on their ends so they grip once in (a good thing, nasty when they have to come out). At least the line itself comes out fairly quickly, easily, and reasonably pain free. Another PICC line was put into my left arm and normal intravenous meds resumed. The sub cutaneous line in my right leg (for the Haldol) was moved to my left arm also which made sleeping on my right side a whole lot easier.
With daily clexane (enoxaparin) injections again, the clot eased after a week and I recognised my hand, thank goodness. I was worried. One nurse /doctor (can’t remember now) had said clots can take three months to resolve. I’m still on the clexane but there are few visible signs of the clot now which is reassuring. Just bruises and quite a few of them. Hey, that’s completely manageable so I’m grateful.
A day in the life while in hospital
11pm – finally finish all the intravenous and sub cutaneous meds for the day. With two exceptions 1) haloperidol and something else in a slow driver which continues to provide anti-sickness properties through the night, and 2) TPN – essentially food and minerals delivered over 24 and 48 hour periods into my PICC line (because I wasn’t eating enough especially through the e.coli business. I couldn’t stomach the fortijuice and shakes that were on offer (pun intended!)
2am observations done – blood pressure, oxygenation level and temperature
Between 5am and 6am – more observations and then the intravenous drug regime and oral meds process began. Some meds couldn’t be dripped in at the same time so I would end up doing one hour of something then a flush of saline (or similar) for 10-15 minutes then 30 minutes of something else and then a flush and then two meds at once for an hour (all while the other two described above kept going in!
This would continue for the rest of the day; obs and meds pretty much until 11pm and the cycle would start again. Sleep at night was fleeting.
I showered on good days and confess to going four days without a proper wash! I can’t even imagine it, yick! When you are sick you are sick! I lived in Hubby’s boxer shorts and a singlet. I didn’t care who saw me pacing the ward (on good days) in these. Staff have seen worse and the get up was the coolest and most comfortable thing to wear. Hubby was an angel – delivering freshly laundered clothing, drinks, whims (shortbread) whenever I asked and that meant most days.
Each time I was woken up I’d need to drink, slowly make my way to the loo with Harry; my Med stand with four pump boxes on it to manage each drug and boy could he bleep. Then back again for the next wriggle up the bed in to a semi comfortable spot and before letting a very patient nurse begin the next hook up! Harry’s bleep would be every time an infusion was 5 minutes from finishing, then once finished, then whenever one of the pumps got it into its techie bits that there was a downstream occlusion i.e. there wasn’t but I may have moved my hand a fraction so it decided bleeping until it was checked was a cautious thing to do. In the end I got sick of buzzing for Nurses who had better things to do and would turn the bleeps off myself and restart the infusions when I was sure a pump was being over sensitive. Anything to stop the bloody beep!

Harry’s mate keeping an eye on me.
Hospital food is beige. I get they try and have a lot of people to accommodate. If you have no appetite and are trying to force yourself to eat; the menu is not a pleasant thing. I did however live on tuna and mayonnaise sandwiches when I was up to it and the kitchen staff were lovely.
Funnies and daft things people say to you
On my second to last day I took Harry to the loo as usual only to realise I wasn’t hooked up to him anymore. That was one image I could have saved him from!
You’ll be out before you know it (when I’d already been in 3.5 weeks). Actually I will know it. I’m willing it. Now I’m begging for it.
Oh I’m sorry. It will grow back quickly (referring to my hair and shaved head). Why are you sorry? I’m not sorry. I’m cool with it. I have more things to worry about than my hair!
Do you have kids? No??? It’s not too late. Oh yes it is!! Its ok my life can be complete without kids. Just because you have five and want more (pity your wife possibly?) doesn’t mean I need to have them.
By the way my responses stayed in my head and instead I would just smile.


First night at home
I’ve been awake since 4am, walked into the garden and around it about six times, felt the rain on my scalp and face. Read a fabulous big magazine (gift from a neighbour and the publisher). Check it out here:
https://www.instagram.com/documentjournal/
https://www.documentjournal.com/
I have revelled in cuddles, kisses, touches, smelling and touching hubby. Holding hands is so special when you haven’t been able to do it for four weeks.
Acknowledgements
Images:
Me & Hubby
Photo by CDC on Unsplash – ecoli style
© 2020 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Blood Clots, E.Coli, Myeloma Treatment, Psychology for Cancer, Stem Cell Transplant SCT, Symptoms and Side Effects Tagged with: Blood Clot, Bone Cancer, Cancer, Chemotherapy, e-Coli, Fatigue, Mucositis, Myeloma, Psychology, Treatment, Worry

Peripheral neuropathy. A fancy pants way of saying pins and needles. Except it is a bit more than that and the more, is scary. When tingling on the soles of my feet and in my hands turned to prickles and cried out for attention, I had just started my 14th cycle of chemo. At night, as if hedgehogs at a rave, the prickles began dancing around, keeping me awake. My self congratulation for having coped well so far and immense gratitude to my body now seemed a little premature or at least to have jinxed me. A strange oscillation between numbness and pain set in. At first, it came and went so I wasn’t too worried. I kept up the once a week, Maintenance Chemo.
Pain
The pain got worse. The tingling turned to a sharp micro needle feeling and the ache crawled up my left arm. I remember thinking, this isn’t good. I started talking to hubby about wondering whether the benefits of chemo still outweighed the side effects. We decided they did. I kept going.
So, did the sensation and the pain. The cannula insertion became excruciating. The drip of the drug into my forearm was ok but by the end of the treatment the whole arm throbbed; I hadn’t had that before. In the days in between chemo, the pain, numbness and needling rollercoaster, deepened and didn’t let up. I felt increasingly fatigued, distracted and unable to concentrate. Pain will do that. The symptoms eased a little if I did nothing and stopped using my hands altogether. Have you tried that? It is nigh on impossible! My weekends became slow, sedentary, dull; low mood came a calling.
Peripheral neuropathy doesn’t like hands
Then it hit me; the way I hold a pen had changed. The length of time I could hold a hairdryer and the way I used a hair brush had changed. Whenever a cap needed to come off a bottle, I now ask for help. I was using two hands to open doors or press flush buttons on toilets. Cooking had virtually stopped (and I had thought I was being lazy) instead lifting chopping boards, holding pans, taking roasting dishes out of the oven were difficult. I no longer enjoyed being in the kitchen. No wonder I’d started avoiding it. Hubby rattled off a list of other things I’d stopped doing or was doing differently.
I felt exhausted just thinking about it. Should I stop treatment? Should I keep going? Would I lose the use of my hands if I continued with chemo? What would life be like if I couldn’t use my hands? If the pain was too much? Was I being a wimp? I’m on a clinical trial, I signed the forms, I committed to it; could I simply stop? What would happen to me if I did stop? Would my cancer flare? Was chemo worth it? Was chemo making things worse? How do I decide whether to continue something that may extend my life, when it seems to be significantly reducing, the quality of the life, I have left? My brain; the whizzing and often unhelpful thought production machine, joined the rave.
Holding pattern
I told my oncologists what we had noticed about the difficulty using my hands and how I was questioning whether to stay on the trial; questioning whether more chemo was the best thing for me. They ran a few tests and determined I had lost strength in my hands, especially my left hand. They recommended I defer chemo for a week.
That week came and went with no improvement. I went into a holding pattern for another week. Peripheral neuropathy is the pits and as well as dancing needles it feels like being burnt, a searing. The pain was constant, in my shoulder, my forearm and using my hands made everything worse. More MRIs were ordered. I started to worry about new lesions. Was it peripheral neuropathy? Would it get worse? Was it something else?
Deal or no deal
It came down to one week and the limit of missed weeks allowed when on the trial. I had happily missed a few weeks of treatment to be with Mum during part of her radiotherapy and then missed additional weeks while we waited to see if the pain and hand function would improve. We now had to decide, the medical team, hubby and I, the best next step for the one remaining week; chemo or no chemo. Sounds like deal or no deal except there was no money involved, no windfall or good luck, instead hope or no hope. Bones versus hands.

Hands won. Living rather than life, won. This time. Drs L and A recommended I stop chemo; they didn’t want my hands to get worse and so I was kicked off the trial.
After 21 months, 17 cycles of chemo, virtually weekly blood withdrawal, 100 odd cannula insertions…it was time to give the body a break.
Care as Usual
I went off the trial and on to ‘care as usual’. What I didn’t factor in, was that meant I would no longer be looked after by the trial team, the team that had had my back from the beginning, the team I had come to know, feel safe with, could express my fears and questions to and laugh with. I would be losing the team that had been with me since March 2017 when I first stepped into the Chemo Day Unit and steeled myself for the uncertainty of cancer treatment. Sigh.
Then of course there were the dominos. The other life challenges, falling thick and fast. Not sure what I mean? See my last post, Silent Dominos.
So while still dealing with Mum’s recovery and ‘what next’ (she’s amazing by the way) and my peripheral neuropathy and hand malfunction… along came the next three dominos:
- Changing treatment, care team and feeling cast out into a new uncertain hospital process
- Dad’s Melanoma came back
- My cancer got worse
Who on earth had it in for my family? Who had we unintentionally, unwittingly, annoyed?
All of us with cancer. At the same time.
We didn’t deserve this. No one does. I needed to remind myself:
Cancer doesn’t care who you are or what you have or haven’t done. It’s simply not that choosy.

Posted in Cancer in my family, Chemotherapy for Myeloma, Myeloma Treatment, Pain, peripheral neuropathy, Symptoms and Side Effects Tagged with: Cancer, Chemotherapy, feet, hands, Myeloma, peripheral neuropathy, pins and needles, Side effects, Treatment

June 20th, 2018 by Janine
A fire has started at the bottom of my ribs. It caught hold in an instant. Creeping upwards, slowly at first but I know what’s coming…it’s picking up pace…then whoosh; my chest, head, face and whole body is washed with heat. Fever type heat, taking over the lymph nodes, my forehead, my entire skin. All my sweat glands are working overtime and can’t compete, they give up. It’s a hot flush or flash and boy is it flashy. It makes its presence known.
Now, I’m hot and wet. Nup. Not that kind. The kind where you feel grubby, like you need a shower and a change of clothes. The night sweats are the worst (well for heat), waking up absolutely drenched, the bed linen soaked and feeling too hot to sleep (if I had any in the first place) …and knowing it will happen again in 10 minutes or an hour (if I’m lucky).
The worst is when you get up, feel good, have a shower, do your makeup, still feel good and then while you are finishing off drying your hair or just as you leave the house or need to head for a train…. whoosh it happens again…. that good feeling a distance memory when frustration, feeling stinky and in need of a second shower takes over. Decisions; go out sweaty or be late and have another shower. Lovely. Stinky wins most of the time. I hate being late. I feel like a woman of the Victorian age as I spray myself with perfume to cover up the body odour.
Mid-life crisis or Climacteric or ?
Speaking of ages and eras, I googled menopause and synonyms came up; maturity, mid-life crisis, climacteric, grand climacteric (no less), matureness, post maturity. Mid-life crisis – what an unhelpful way to talk about menopause. Though finally and slowly, Menopause is being talked about (mind you, we could do with a royal to take up the band wagon and bring it into the bright light). Climacteric is an interesting one, apart from referring to Menopause in medical circles it also denotes a critical period or event and having extreme and far-reaching implications or results. I got a shock when I discovered what some of these far-reaching implications were. Men, this is just one of the places where you come in!

Shock
In the week when I decided to research Menopause and Cancer the universe must have been aligning; three different sources of Menopause information happened into my path. The first one; I turned on the radio and heard the presenter say a piece on Menopause was coming up. Perfect timing.
Menopause; a completely natural process involving women’s bodies producing less oestrogen and changing progesterone hormone levels. I’ll come back to the implications of these in part two of this blog. For now, let me tell you about something I heard on the radio that shocked me. The host talked of how she had discovered some high flying, dynamic women at the top of their career had left their jobs due to the difficulty they had experienced in managing the symptoms of menopause.
Shocked doesn’t really explain it. In this day and age? I didn’t doubt that the symptoms must have been horrendous; I was stunned that women were not being adequately supported by medicine or natural means to enable a normal physiological transition to be facilitated so that their lives and work were not impacted in such a significant way. The feminist in me wondered if men would have put up with this state of affairs though to be reasonable, menopause appears to be a learning curve for many of us. Consequently, I was shocked.

I was even more shocked when men joined the discussion and explained their relationships had broken down, divorce had resulted and they described their many regrets about not having understood what the women in their lives were going through during menopause.
Job loss, love loss. OMG. Menopause, you can be incredibly cruel and we need to talk about you, a whole lot more. Now!
Symptoms and Years
In my humble opinion, Menopause symptoms are sh*t: mood swings, hot flushes, night sweats, brain fog, short term memory loss, difficulty in finding words and string sentences together, fatigue, low libido and vaginal dryness. They often start when women are in their 40s and 50s though can start when women are much younger.
Symptoms often last YEARS. Men, please note this. YEARS not weeks or months. Most women (8 out 101) face life impacting menopause symptoms for between 3 and 7 years and for some women, the rest of their lives. On top of this, perimenopause (the few years before menopause starts) usually brings unhelpful, generally unwanted symptoms too including disrupted sleep, headaches and heavy periods.

Ok, not all women experience these symptoms so we must be careful of making assumptions however MOST women do find themselves having to go through yet another massive learning curve about their body. And guys, it would be great if you came along for the educational ride. Not least because men go through a ‘pause’ of sorts too!
For men, it’s called andropause and refers to age-related changes in male hormone levels. Male menopause (not necessarily a helpful term) involves a drop in testosterone production in men who are age 50 or older. It’s often affiliated with hypogonadism. Both conditions involve lowered testosterone levels and similar symptoms.
You’re getting on my wick…
Ha. So we DO have an excuse for being irritable and bitchy. Sort of…well, not really…because it’s not that helpful, is it? Usually most of us just feel worse when we let irritation get the better of us and say or do something we wish we hadn’t said or done. However, when we know hormones may be playing a big part in our mood we can use our awareness to catch ourselves in our irritation and then choose our words and actions carefully, with more sensitivity. Not always easy but likely to result in a better day. It’s also OK to acknowledge we are feeling easily irritated!!
The more we talk about menopause, the more men and women will be able to identify when peri-menopause and menopause start. We can then learn about the options for managing the unhelpful symptoms. Finally, both men and women can then practice and take responsibility for being supportive, tolerant and understanding of each other and ourselves as we go through these changes. Maybe then, we’ll be able to avoid mountains from molehills and the extremes; relationship challenges and break down, negative outcomes for career and lifestyle.
Now imagine dealing with all of this…and cancer…and chemo.
Except, there’s more.
Identity
I wish it was just the symptoms listed above and the frequent embarrassment that accompanies them, that many women were dealing with. Going through the menopause can play havoc with women’s sense of identity, sexiness, and value in the world. Western society still predominantly relates to the menopause phase as women becoming old and somewhat invisible rather than being mature, loving and fully living life.
Edna M. Astbury-Ward summed it up well in her 2003 paper
The social construction of menopause as the entry point to old age may represent a challenging and difficult time, because while women may feel young, society tends to perceive them as rather less attractive and less fully functioning. This perception of menopause as a negative milestone is often found only in Western cultures. Medical culture also influences the meanings of middle and old age, particularly for women at the time of approaching menopause.
Cultural bias against ageing and sexuality has contributed to that stereotyping of older women as asexual. In general, the media has not served the ageing female well. Older men are often marketed as sexy, yet older women are rarely seen outside of advertisements for hormone replacement therapy (HRT) and Conti knickers.2
I suspect we need a new, positive and helpful narrative for the completely natural yet often difficult to go through transition that is menopause. The recent menopause cafe phenomenon may be helping with this as a space is provided to discuss menopause and challenge stereotypes.³ Princess Anne, Duchess of Cambridge, Kate; Duchess of Sussex, Meghan – you don’t fancy taking up the band wagon, do you?
Chemo vs Menopause
This was the backdrop to my realisation that chemotherapy and menopause symptoms are eerily very similar. I had been struggling to manage some of the chemo symptoms, particularly the lack of good quality sleep yet they may not have been chemo side effects at all (or at least not current side effects).
My next challenge along this cancer journey was now starkly obvious; to work out how best to support myself over the next year of treatment or to review treatment options, I needed to discern what was a chemo symptom and what was a menopause symptom and then learn how to address each in the best way for me. In the back of my mind it also occurred to me that I may end up going through this whole process twice so getting a handle on it was crucial to enjoying my life and living it to the full. Twice, because my menopause was possibly chemotherapy induced and not following its natural path. I was yet to find out if there was a chance my symptoms would stop then start again once chemotherapy was complete (joy of joys).
There it was, a whirlpool of thoughts swirling around, when in the space of a few days, I turned on the radio at the right time, walked into a foetal medicine building to use the loo only to discover a medical exhibition on menopause and noticed a webinar series advertised on social media involving a week of interviews where experts in menopause shared their pearls of wisdom.
Timing and attention; thank you, Universe.
Part two coming up -– the nuggets from the Menopause experts and my oncologists’ stand-off!
I am going to take a breather now… oh, and another shower.
References
1 https://www.nhs.uk/conditions/menopause/symptoms/
2 Astbury-Ward, E. (2003) ‘Menopause, sexuality and culture: Is there a universal experience? Sexual and Relationship Therapy’. Journal of the British Association for Sexual and Relationship Therapy. 18(4), 437-445
³ https://www.theguardian.com/society/menopause – Menopause café and challenging stereotypes about aging.
Acknowledgements
Images: Unsplash:
Steam_skyler-king-527288;
Shock_andre-guerra-676198;
Divorce_rawpixel-666933;
Sleep_vladislav-muslakov-261627
© 2018 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Menopause, Myeloma Treatment, Symptoms and Side Effects Tagged with: Cancer, Chemotherapy, Menopause, Myeloma, Side effects, Treatment

I’d be pulling my hair out over the steroid incident (see last post) or I would be, if it wasn’t falling out, on its own accord. I’d be pulling my hair out over this week’s incident: a miscommunication between the Clinical Trial team and the Lab that makes up my chemo drugs resulting in me having to wait an extra three hours, until after 5pm, to be hooked up and receive my treatment. I didn’t get home until late and that meant less recovery and down time than I usually have on a Monday. Well, I would be pulling my hair out over this, if it wasn’t already receding at what seems like a rapid rate and coming perilously close to exposing my devil’s horn. I only have one (maybe I do things by halves after all!) bump of calcified bone formed from hitting my head a million times over my life time: on open cupboard doors, someone’s elbow when standing up, fridge doors, you name it I’ve managed to bump that same place on my head in some extraordinary ways! Hair loss and receding hairline, missed steroids and treatment delays. More, thank you Chemo, moments.
I know I’ve been lucky: I started with a lot of hair. A lot! Unlike many people going through Chemo for breast cancer and cancers other than Myeloma, my treatment is not usually linked with complete hair loss. I would not be a sexy bald (though have decided to do my best to embrace it, if it does happen). It is stressful to see the masses of hair come out in my fingers, in the sink, in my brush, in the air.

Hair loss – today’s right hand scoop – a light day (yay!)

Hair loss – today’s left hand scoop – a light day (yay!)

Hair loss – today’s offering
I’ve lost about a third of the volume so far. My hairdresser K, who I’ve known since 1993 (longer than my hubby and my ex!) knows my hair well and confirmed I wasn’t dreaming this. I am fortunate: I have regrowth already. Well lucky of sorts. The regrowth is crazy curly and goes out at right angles. Hubby nicknamed my curls, Turkey Twizzlers. Helpful. Giggle.
With my hair down, things are hidden and a bit tidier but the odd curl makes its way out over the day and spooks me when I look in the mirror – how long has it been jutting out like that ???!! OK curls can be cute (very very beautiful in fact, like those that adorn my sister-in-law and gorgeous niece) however a whole heap around my face when I am used to waves and straight hair takes some getting used to (as I imagine being bald does too). The curls are also resistant to smoothing serums and are frankly unmanageable. I give up. I hope they hurry up and grow long so gravity straightens them out.
Growing. Regrowth. That’s a good sign, isn’t it? The Chemo can’t be killing off all the good cells. Surely my nails and hair wouldn’t grow if my body didn’t tolerate the Chemo well, most of the time at least (and when I get my steroid on the right day, not bitter, can you tell?!). My nails, will I jinx them saying this? They seem super resilient so far… I hope it lasts. For the first time that I remember, my results show I’m calcium deficient so now I’m on an extra tablet for that and reintroducing halloumi and mozzarella.

New Curls
Sticky eyelids and thin skin
Hair loss, sticky eyelids, thin skin that leads to blisters or adhesive grazes when they wouldn’t normally occur are just some of the small and large niggles cancer and chemo have added to my life. Sticky eyelids are frustrating…I’m constantly pulling at my lashes to ‘release’ my eyelid from my eyeball. Refresher drops help a little though the stickiness quickly returns. Are there any advantages to sticky eyelids? I can’t think of any? Do let me know…
I put on a favourite super comfy pair of boots and invariably on a day when I’m running for a train or having to do loads of walking, five minutes in, I have a blister. Pre-chemo I wouldn’t have had a blister – its why I put these boots on after all! Scrabbling around for plasters, hoping they’ll stay on, too late, damage done, now nothing works. I revert to trainers as soon as possible.
Anyway, back to hair. What to do? Regain has been suggested. K has told me some of his clients also living with cancer have had great success with it though its best started as early as possible. What do you think – should I give it a go? I suspect it would possibly be introducing a toxin however is it a worthwhile trade-off? Every week there is something new that I think needs my attention and involves time consuming research yet if I don’t do it, I feel like I’m not doing the best I can do. It’s so exhausting.
Psychology
Body changes
Changes in body image will take getting used to and as always require kindness and compassion. It can be helpful to look in the mirror and look for what I love and am grateful for and not just focus on the unwanted changes.
For some people, hair loss is one of the most difficult aspects of living with cancer treatment as it can be entwined in their personal sense of self, preferred way of presenting self to the world and identity. It can also be tied up with ideas and assumptions about what it is to be feminine, masculine, young, virile, strong and attractive to others. Hair loss can trigger anxieties or trauma associated with earlier life experiences where people received unhelpful comments about the way they looked.
Society influences about what hair should be like overall, or at certain ages or what a hair style represents can also trigger unhelpful assumptions, rules and thoughts such as I must cover up my baldness, no one will find me attractive, I’m no longer feminine/masculine therefore there is no point being open to a new partner, friends won’t want to be seen with me so I shouldn’t meet up with them.
Hair loss and anxiety relating to hair disorders can be extremely distressing for some people…however you do not need to put up with it. Talking therapy with a psychologist can help with the distress. Therapy can help you uncover your thoughts and feelings about your hair and image, discover what is helpful and unhelpful, what is keeping distress going and identify new strategies to try out that nurture your identity, social interaction and self confidence. Therapy can help you accept your new or current image and not be stopped by any unhelpful thoughts about it.
Trichotillomania and Alopecia
There are many other difficulties relating to hair that people live well with live every day. Trichotillomania and Alopecia are just two of those. For those that experience great distress about these talking therapy can also help in similar ways as described above. If distressed, if one of these conditions is stopping you feeling like you or doing the things you want to do – don’t go it alone – a psychologist can help.
Trichotillomania (trik-o-til-o-MAY-nee-uh). Sometimes referred to as hair-pulling disorder, is a mental disorder that involves recurrent, irresistible urges to pull out hair from your scalp, eyebrows or other areas of your body, despite trying to stop.1
Alopecia and Alopecia areata. Alopecia refers to hair loss generally while alopecia areata refers to a specific, common cause of hair loss that can occur at any age. It usually causes small, coin-sized, round patches of baldness on the scalp, although hair elsewhere such as the beard, eyebrows, eyelashes, body and limbs can be affected. Occasionally it can involve the whole scalp (alopecia totalis) or even the entire body and scalp (alopecia universalis).2
Mental Health Awareness Week
By the way – It’s mental health awareness week in the UK and this year the focus is on stress. More about it here https://www.mentalhealth.org.uk/campaigns/mental-health-awareness-week. Talking about mental health helps to reduce stigma. I know I’ve said I don’t always welcome being asked ‘how are you?’ however that mostly related to diagnosis and early treatment days of living with cancer. I encourage you to tell someone how you are feeling. If you can ask someone else who you suspect may be feeling low or anxious or whose behaviour has changed (they’ve become more withdrawn, don’t seem to enjoy the things they used to enjoy or you notice appear to be struggling) if they want to talk. 5 minutes can make a huge difference. You don’t have to say anything special, just listen, acknowledge what they are saying and help them understand they are not the only ones to feel that way.
I know this because I work with people every week who share their experiences and symptoms. Research tells us1:
- Worldwide – Major depression is thought to be the second leading cause of disability worldwide and a major contributor to the burden of suicide and ischemic heart disease
- UK – Approximately 1 in 4 people in the UK will experience a mental health problem each year
- England, 1 in 6 people report experiencing a common mental health problem (such as anxiety and depression) in any given week.
- USA – Approximately 1 in 5 adults—43.8 million, or 18.5%—experiences mental illness in a given year.
- Australia – Almost half of the total population (45.5%) experienced a mental disorder at some point in their lifetime
- NZ – one in six New Zealand adults (16%, or an estimated 582,000 adults) had been diagnosed with a common mental disorder at some time in their lives.
Each person’s circumstances and road/process of recovery and managing mental ill health may be different yet there are often commonalities of impact on lives and symptoms.
Just imagine, this week might be the week you seek help or offer help to someone living with stress or living with the stress of cancer. What a difference you will make maybe without even knowing.
Then think of me with a Donald Trump style comb over. IT IS NOT GOING TO HAPPEN!
References
1 https://www.nhs.uk/conditions/trichotillomania/
2 http://www.britishskinfoundation.org.uk/SkinInformation/AtoZofSkindisease/AlopeciaAreata.aspx
3 see Mind and Mental Health Foundation and National Health Alliance on Mental Illness, Australian Government – Department of Health, NZ Mental Health Foundation for references and other details
Acknowledgements
Images: Upright Hair – mohamed-nohassi-531501-unsplash & Me
© 2018 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Psychology for Cancer, Symptoms and Side Effects Tagged with: Alopecia, Alopecia areata, Cancer, Chemotherapy, Hair, Hair loss, Myeloma, Psychology, Receding hairline, Side effects, Sticky eyelids, Trichotillomania

February 22nd, 2018 by Janine
Dr L turned to his colleague and said, ‘for someone with Myeloma, Janine’s immune system is a Schwarzenegger’. Hey Arnie, you are now a metaphor for my health status. Who’d have thought?! It sounds so positive and I am very grateful that my precious physical self is coping so well with the toxicity of Chemo. I notice too that I get a little hung up on the ‘for someone with Myeloma’ phrase though more about that in the next post. Now, I want to talk about my relationship with my body. It has become a bit confused.

Can I share a secret? I liked it when cancer, chemo and a diet change caused me to lose weight. I like being closer to 60kg than 70kg. I like how slim and less pear shaped my legs look. I like being size 10 and for a few weeks, size 8. All my life, I have valued being slim, strived for it. I’m not obsessive. I don’t over exercise or starve myself or think about it constantly. Even when I put on two stone from IVF treatment: I hated it but didn’t panic. The weight had context. Once we stopped IVF treatments, I lost a stone quickly and then worked on chipping away at the rest. I like cake. I binge occasionally (or did before this new eating regime). Who doesn’t when there is a pack of dark chocolate hob nobs in the house and the hormones are taking over? I would say I’m weight and health conscious with no extremes.

I’ve never liked my arms: they’re too big. Well, apart from the time I sanded every spindle on a stair case by hand: my arms were toned, like Madonna’s or Geri Halliwell’s. I thought my arms looked great after that. It didn’t last long. Finding tops and elegant shirts to fit my arms has always been a hassle. The welcomed side effect from cancer, chemo and clean eating has been the slightly thinner arms and shirts fitting, for once. I don’t really want to give that up yet…
I find myself struggling. I’m in a tussle inside my head. Too much weight and muscle loss is not healthy, not helpful and goes against Dr L’s advice. He explained that he had noticed that people with Myeloma who keep up with the gym and have some muscle reserve seem to manage the chemo better. I do want to live as long and as well as I can. Yet I find myself loving my new size. I bought a pair of boyfriend jeans a few months into treatment, laughing with a wave of pleasure when I discovered I could fit into a size 10 only to find they slipped off a month later and I’d lost even more weight. Now what do I wear? Nothing in my wardrobe fits!!
At that point, 61kg, it did get a bit worrying. My face was looking drawn. My rib cage and spinal vertebrae were a too visible. I promised Dr L that I wouldn’t let my weight fall further. I expanded my food repertoire slightly (good quality bacon, goats cheese, sourdough toast occasionally) and started the weight training.

Back at the gym, I felt good and waves of relief from feeling stronger. I’d become so weak. I was asking hubby to open jars and water bottles for me and lift anything. This does not fit with my independent and equality philosophy. Yet, I dislike how quickly my leg and arm muscles grow. When my weight started to rise slowly I would find it hard to like what I saw in the mirror. I know it may seem silly in others’ minds. Intellectually, I know I look ‘normal’, ‘healthy’ and would still look heathy even if I did put on weight (I’m fortunate to be tall). Except, somehow it feels like a tug of war in my brain – Janine, don’t put on more bulk, you look good as you are (now size 10-12) versus Janine, you need more muscle and strength to manage Chemo effectively, get yourself to the gym.
For more years than I care to think about, I have gone to buy clothes and come back disillusioned when I have needed that elusive size 13 or 15. It seems crazy to have the same problem at a lower size (now 9 or 11) and with the added complication of my size constantly changing. I can’t afford and wouldn’t want to invest in new sets of clothing every few months yet as my weight goes up and down on chemo, what can I do? Frustrating. I hate being uncomfortable in clothes. I really dislike ill-fitting clothes that don’t help me feel good and enhance how I look in the world. Too loose is as bad as too tight!

Even more annoying, last summer, before diagnosis, I bought some new clothes after ‘making do’ for a few years. Now they are sitting in the wardrobe, barely used as they are far too big. I am in the maintenance phase of treatment, with 3 days rather than six days a month of Chemo and my weight is climbing and fast. I’m 67kg today. Maybe I’ll need those ‘larger’ clothes again in a couple of months. Except, I don’t really want to get any bigger or go back to the size of those clothes again. The 6 days of steroids each month may have something to say about that.
67kg. Nothing to worry about. Yet, I don’t feel good about it. I am beginning to worry that a steroid induced, sharp trajectory up of weight, will set in and hang around for the duration of treatment. There are 16 months to go! That’s a lot of weight gain. That makes me feel sick.
It is also motivating. I’m back on the high veg and protein regime. A few bits of non-clean eating crept in as I celebrated getting through the first 48 (see previous blog) and 9 months of treatment. Then I let the goodies stay, it was Christmas after all. Then I felt sorry for myself with the arrival of two viruses back to back. January came and went, and it’s always the toughest month in UK for me. It’s so often grey, cold, hibernation inducing and all I want to do is eat comfort food!
Oh well, not having the clothes I would like, in the bigger scheme of things, is insignificant really. If I hover around the 65kg mark and I am made of tiny Arnie style muscles, that will be good enough. Viruses and January blues are gone. The revolution is here. February has arrived.
I’m back on track with preventing my body from being a perfect host for cancer. I celebrate a new food focus: FISH. It is easy to do: I am languishing on the beautiful beaches of ANTIGUA for a much-needed holiday. Fresh snapper, mahi and octopus are on the menu. The company is great (hubby and besties), the sun is high, the sea is warm and the forecast is rosy. No time for weight tussles now: The bikini is out and about!
Acknowledgements:
Antigua seascape: Photo by me
Legs and kettle bell: Photo by Maria Fernanda Gonzalez on Unsplash
Clothes hangers: Photo by Christian Fregnan on Unsplash
Shirt and Jeans: Photo by Lyndsey Marie on Unsplash
Muscles: Photo by Alex Boyd on Unsplash
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Finance and Cost, Psychology for Cancer Tagged with: Cancer, Chemotherapy, clothes, muscles, Myeloma, weight
December 6th, 2017 by Janine
What a year! I turned 48, I was diagnosed with cancer and I’ve completed 48 chemo sessions. I love the number 48; it seems so symmetrical to me (I love a bit of symmetry). Now ‘48’ has a WHOLE new world of associations!
Warning…I have happy news, and, I’m going to talk about toilet rituals.
First, the rituals.
This may seem very strange to those of you who have always been super careful about hygiene when using public loos. In my defence, I have rarely worried about these things because my childhood in New Zealand was filled with non-traditional toilet arrangements. When you are fortunate enough to spend all day at the beach or walking in the bush or driving long stretches of deserted road or camping in remote sites you tend to get over yourself quite quickly about going to the loo wherever and however.
Doing your business quickly behind a tree, rock, or in a smelly long drop with minimal paper or alternatively leaves or seaweed, is not that unusual. Worrying about being seen was always a bit more bothersome than worrying about bugs, microbes or possible infections! The upshot is; I have never worried about using public loos, ‘catching anything’ or having to use disinfectant. I just focussed on washing my hands well.

Now that my immune system is compromised it’s another story completely….though maybe I’m being a bit anal? (pun intended)
In the Chemo Day Unit, patients are asked to ‘wipe the loo’ with anti-bacterial wipes before and after use. I recently discovered I had developed a wee ritual…Take a wipe, clean toilet seat, fold dirty side in, use clean side to wipe toilet handle, tap, hand wash dispenser, door lock, door handle. Dispose of wipe in bin. Use loo. Wash and dry hands properly – you know the 8-10 step process (depending on the poster). Take new wipe and clean toilet. Goodness knows what bugs I could pick up if I didn’t do this; don’t tell me!
Anyway, this is a new ritual in my life and once again one that seems to consume a little more of my available time and life though hopefully is worth it. It seems so, so far, as I have yet to pick up any major nasties despite lower immunity and chemotherapy for 9 months now. This ritual has now made its way out of the hospital and into public conveniences. AM I being anal? I’ll let you be the judge!


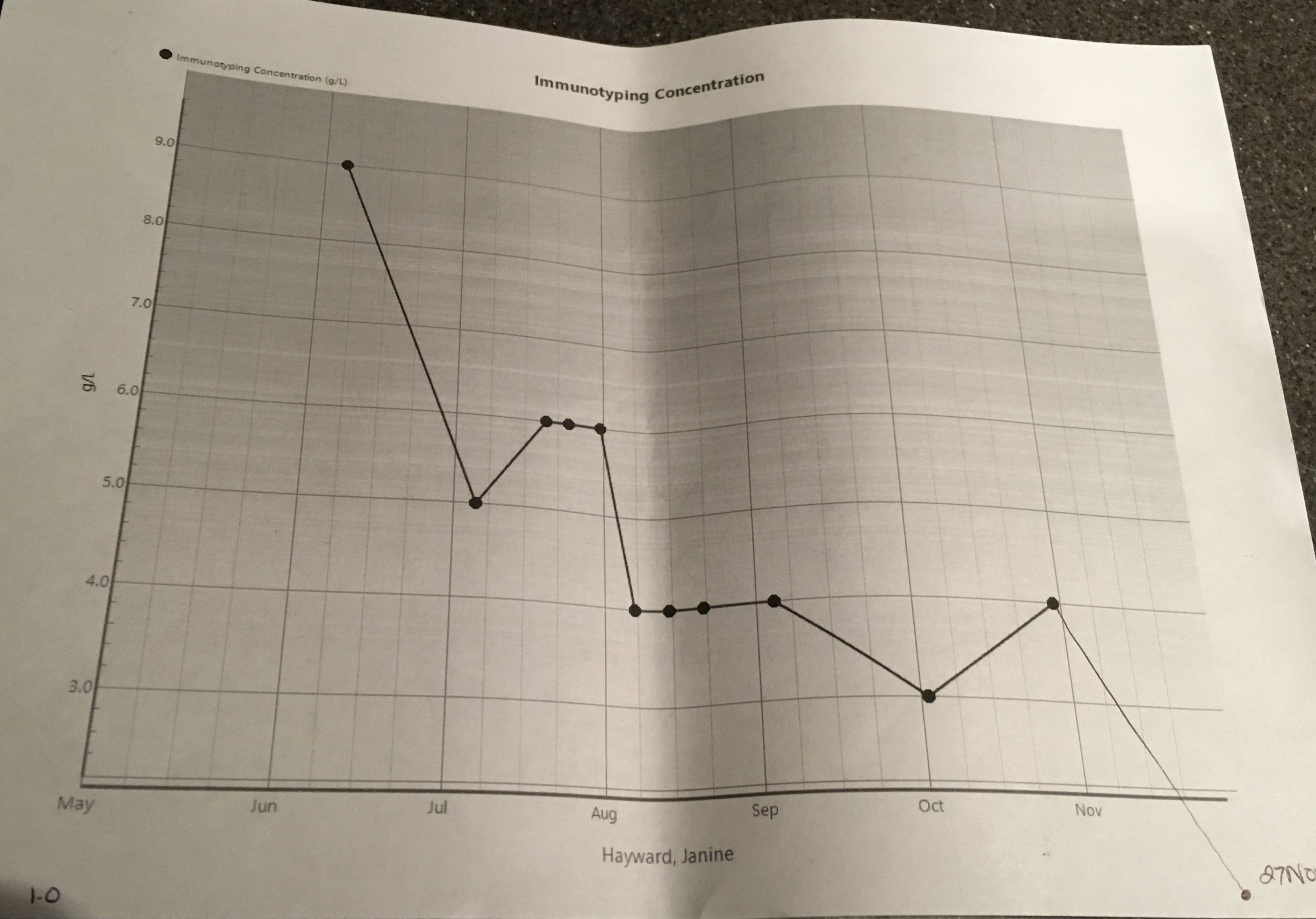
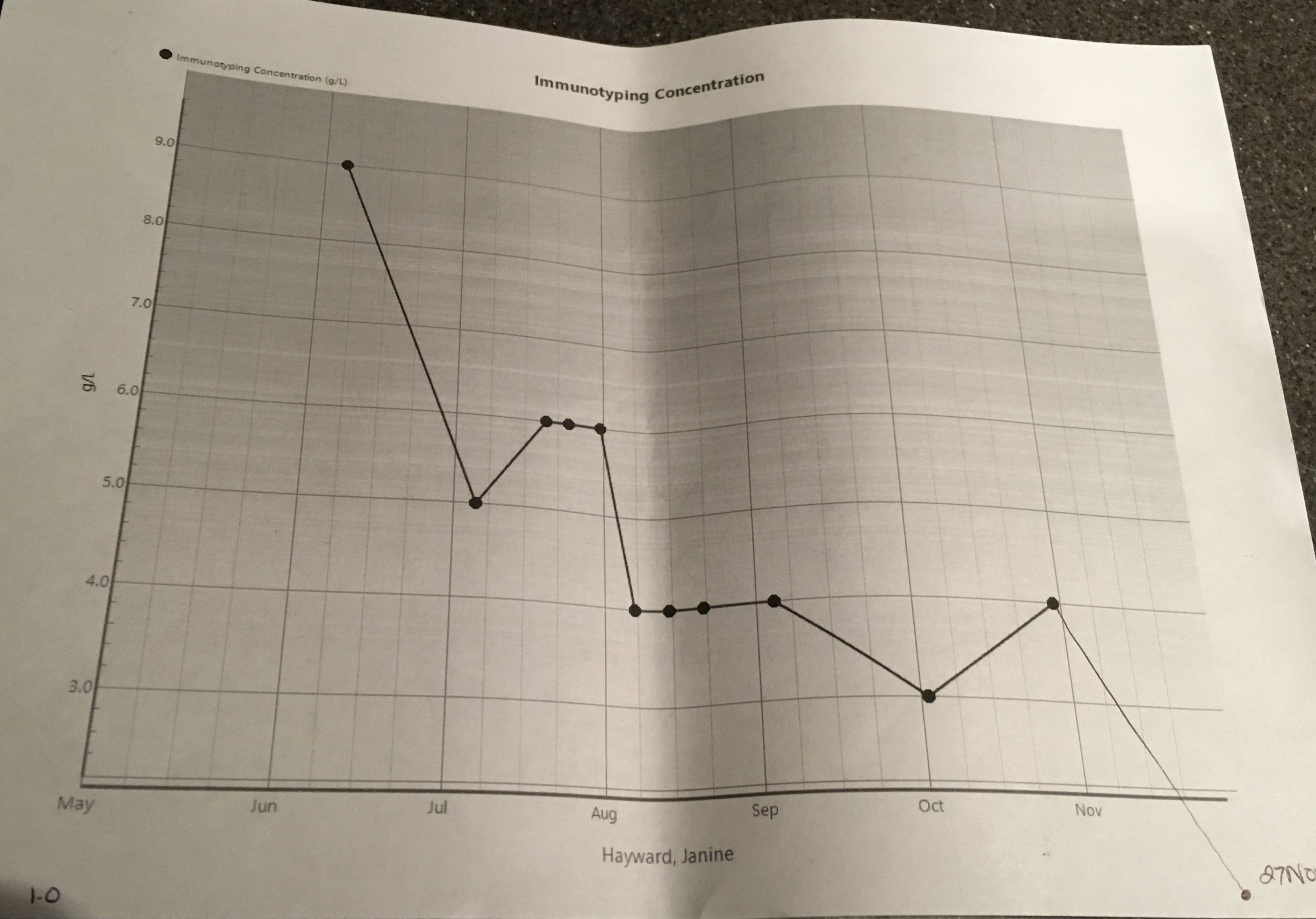
My News
…is happy, positive and hope-FULL…I’m very grateful for it and its effect; a reaffirmation of my faith in my medical team, the drugs and my health and life choices. The Myeloma presence in my body has decreased further in the last few months… It’s down to 1 g/l (42 g/l at its peak) and a may be yet to plateau. Yee ha! Not only that, the serum kappa light chain results are 1.75 mg/l, backing up this great news and described as ‘excellent’ by Dr L. On top of that my liver is doing well. My Hb (Haemoglobin, the protein found in the red blood cells that carries oxygen around) level is back up to 121 g/l so I no longer need to consider taking EPO (yes, the cheaty cyclists’ drug of choice! I’m a tad disappointed. I had wanted to experience how energised I’d feel!) While 121 g/l is lower than the desired normal levels (125 g/l plus) it is great for someone with Myeloma. My kidneys are also doing OK for someone with Myeloma, my Creatinine is 69 umol/L and normal level for women is approx. 45 -90 umol/L (I think; there seems to be some debate!). Lots of good, great news, here. Dr L delivered these details and then reminded me to keep drinking 2-3 litres of water today for kidney care. I imagined my kidneys; bloated, water-logged, bean-shaped balloons, wrapped up in clouds of cotton wool, floating about, relaxed and without a worry in the world.


I’ve had yet another bone marrow biopsy and pet scan (what effect does three doses of radioactive sugar chasing gunk in a year have on one’s body? I guess I’ll find out!). I have an ear numbing full body MRI coming up in a fortnight.
Let’s hope they show (or don’t show lesions at all) that lesions are further dissolved and there are no new uninvited guests!!
What a year.
48.
One number I’ll never forget.
Acknowledgements
Images: Me (graphs va KCH), Long Drop – Sarang (public domain use permission granted)
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Myeloma Treatment, Results Tagged with: Bone Marrow Biopsy, Chemotherapy, Myeloma, Results, Tests, Treatment
It’s been hard to write the blog in week’s four, five and six of Chemo; I didn’t know where to start, there didn’t seem to be time, and I was worrying. Even Music didn’t show up much; I didn’t hear it or go looking for it – strange.

I started to worry about having little time; not time on this earth but time during the day to do all the things I needed to do. Sound familiar? I have learned over the years that when I worry about not having enough time, it usually means I am probably trying to do too much and am not getting enough rest or chill space. I noticed too that when reminders popped up in my calendar to get some ‘headspace’ or do a visualisation, I was swiping them away and thinking I’ll do that later yet later never came. This worried me.
I wondered whether my blood test results for week four would not be as good as the previous weeks and imply that going away to Canada had been a bad call after all. It turned out this worry, while natural, was unfounded; my results showed more test results falling within the normal range than in the previous weeks and suggested my immune system was hanging in there – a good result.
I worried about an interaction with a Nurse and found myself feeling ‘told off’, then wondering if I was being over sensitive, or not sensitive enough to others. I felt guilty for coping well with and doing well on Chemo. The nurse had asked how I was doing and I had said something along the lines of “really well thanks” and “chemo had been quick today”. I heard a response of “well that’s not the case for everyone”.
Then a stream of thoughts flooded my mind;
- Sh*t, had I spoken too loudly?
- A lot of people look very ill and drained on the Chemo ward today, have I not thought of them? Should I think of them?
- I have answered honestly and positively; that’s what I committed to do throughout this process wherever possible.
Feeling a bit indignant, more thoughts rushed in;
- No, it’s fine for me to be positive after all it’s not my fault I’m doing well,
- Being positive is meant to help with healing so I’m not going to stop answering ‘I’m Doing Well’, when I am doing well.
Overnight and with reflection I decided I probably was being a bit sensitive and it was also fine to be positive. The following day I checked in with the nurse, who quickly reassured me that he had not thought I’d been insensitive to others on the ward at all. We cleared any misunderstanding and he reiterated how great it was that I was doing well. This frank discussion helped bring clarity and perspective to my thoughts. It stopped this worry completely. I’m glad I raised it with the nurse even though I was uncertain (and nervous) about what I might hear.

Despite this resolution, a residual sense of stress, worry and an over active adrenal system remained; the opposite of the many calm moments that I had been experiencing last month. The overall worrying continued.
My weight had dropped again to 66kg and I was struggling to eat enough calories. I often didn’t feel hungry but still tried to eat. I hoped my weight would stabilise and even climb back up to 68kg. That weight had felt comfortable while now I noticed I didn’t seem to have much padding, wondered if I really did have much of a reserve if I got an infection and I noticed I had lost muscle mass. The backs of my hands look like some very elderly person’s hands; dry and wrinkly despite the constant fluid intake. I worried that my weight would keep falling and my skin would get worse.
I worried about whether I should stick to the plan of not working for six months to focus on getting to remission as successfully as possible or to work while I still could. I worried about if I worked, would it be too stressful, leave me enough time to rest or feel like it’s getting in the way. I worried about not being able to work out how much work was too much, and for private practice whether enough work matched with breaking even financially. I worried about how to contain my clients’ concerns if my appearance changed with more chemo and how I provide a consistency of safe space for them if my medical appointments needed to change in the future. I worried and yet I missed making a difference and being the psychologist I know I can be.
To cap off the week, I finally had a long-awaited Ear, Nose and Throat appointment (yet another hospital visit) to check my possible hearing loss. This is something else I have been worried about for a long time and that has no doubt been bugging Si for years as I constantly ask him to repeat himself or need the TV volume well above the level he would choose. I had noticed my hearing was worse when; I’d find it difficult in crowded places (and with background noise) to hear the person I was standing next to and speaking with, or to hear what someone was saying if I couldn’t see their face and mouth. I noticed I had started guessing (not always accurately) what someone was saying.
For a psychologist; listening skills are imperative and before listening skills can be invoked one has to be able to hear! While I had rarely experienced these problems in one to one therapy sessions, I was concerned symptoms would get worse or impact my functioning. Sure enough I wasn’t dreaming this either; tests showed my hearing has deteriorated though is still in the mild loss range; inner ear cochlear deterioration so unrecoverable. This is essentially the kind of loss most people start experiencing from around 60 years old on…except I’m not 50 yet! I suspect I’m paying the price for good times; a burst ear drum while scuba diving as a teenager and damage from standing far too close to speakers at Fabric nightclub a few years back (ok, so quite a few years ago now).
So I’ve been worrying and it’s completely natural to worry. It is not helpful to dwell in worry or worry about things I can’t control so how do I let go of it? Worry is something I have helped many clients with over the last ten years so it is definitely time for some self-help. Below are the psychology tips and strategies I reminded myself to use.
Psychology – Overcoming and managing worry

What is Worry? How worry works.
Worry is a form of mental problem solving about potentially negative future events. It can be triggered by a variety of external events or from thoughts that just pop into your head. Worry is characterised by a lot of ‘what if’ questions. For example, ‘What if my Chemo doesn’t work?’ ‘What if my new boss doesn’t like me or think I’m good enough?’
Normal worry is usually short lived and leads to positive problem solving activities. Worry becomes unhelpful when it is about several things, is frequent and difficult to control or dismiss. We can think prolonged or frequent worry helps with problem solving, planning and preparation however worry breeds more worry (and anxiety) which prevents positive thinking and action.
Worrying can rob people of time. It’s exhausting and often leaves people feeling tense, with disturbed sleep, difficulties concentrating, and feeling irritable. While sometimes it can feel appropriate or necessary, worrying is exactly the opposite; it’s restrictive, and takes up time, attention and energy that could be spent on useful, enjoyable and meaningful activities.
Why do some people seem to worry more than others?
Worrying is human! The causes of are not clearly understood though it may be that a number of vulnerabilities increase the chance of developing a tendency to worry excessively; prolonged stress, past experiences of uncontrollable or traumatic events, an inherited biological disposition to experience negative emotions, learned messages from others that the world is unsafe or that worry is useful, and a coping style that involves avoiding challenges or situations where there is a chance of experiencing negative emotions (which prevents positive experience of coping and positive emotions).
Managing worry.
UNDERSTAND YOUR WORRY CYCLES – Understand your vicious cycles of anxiety and how avoidance contributes to anxiety. See the handout below (CCI – Vicious Cycle of Anxiety).
NOTICE YOUR PAYOFFS AND COSTS. Part of understanding your worry can be to notice if you are getting a pay-off from worrying, ‘buying into it’ and most importantly what the cost of the pay-off might be. Are you avoiding going out? You might get a pay-off of avoiding any negative emotions such as uncertainty of what will happen or be said when you see someone but you also miss out on the potential positive experiences; fun, laughter, connectedness or ease which going out may also provide. Also notice, where do you worry and what are you doing when you worry. For example, are you sitting down and telling yourself ‘you are worrying but getting rest at the same time’. Consider that your type of ‘sitting down’ in this instance is not truly restful and what it actually costs you is feeling rested. If you shifted your attention away from worry to giving yourself permission for genuine rest, and allowed yourself to do something enjoyable without the worrying in that same time, you are much more likely to feel rested and relaxed (and be better able to cope with normal levels of worry that we all experience).
Other practical strategies:
USE A WORRY TREE to identify where to put your attention so that you shift your attention to worries you can do something about and form a plan for rather than worries you have no control over. There is a link to a handout below
CHANGE “WHAT IF’ STATEMENTS TO ‘HOW’ STATEMENTS’. For example, instead of “what if Chemo doesn’t work?’ I might ask myself ‘How will I act if Chemo doesn’t work? How will I find out what action can be taken next?’
POSTPONE WORRY. This is where you give yourself permission to worry about a specific topic, at a particularly time later in the day, for a maximum duration of say 20 minutes). This way you are acknowledging your concern and allowing yourself to think about it for a contained amount of time without it taking over and impacting the rest of your day. Sometimes you may find the thing you were worrying about has resolved itself by the time the allotted worrying time has come around, or it looks completely different and isn’t as big of an issue as it seemed earlier or doesn’t have to be dealt with today after all.
Summary
These are just some tips for managing worry and there are others if these don’t work for you. Remember, while worry is normal, excessive worry can be gripping and creep up on anyone. Even when worry can feel like a good thing to do, it creates more anxiety. When it stops you from enjoying life or doing the things you want to do, worry is not your friend. Excessive worry can be overcome. Please try the strategies outlined above and the links to helpful handouts below. If you find them hard to do alone, do talk with your GP or ask a psychologist to help with gaining treatment or to work through the strategies with you.
Acknowledgements, Permissions and Helpful Handouts:
Centre for Clinical Interventions (CCI), Department of Health, Australia http://www.cci.health.wa.gov.au/
CCI Generalised Anxiety and Worry
http://www.cci.health.wa.gov.au/resources/infopax_doc.cfm?Mini_ID=46
CCI Vicious Cycle of Anxiety
http://www.cci.health.wa.gov.au/resources/docs/Info-Vicious%20Cycle%20of%20Anxiety.pdf
CCI Postponing Worry
http://www.cci.health.wa.gov.au/docs/ACF3D66.pdf
Get Self Help Get.gg – Worry Tree
https://www.getselfhelp.co.uk/docs/worrytree.pdf
Images: Simon Hayward
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Psychology for Cancer Tagged with: Cancer, Chemotherapy, Myeloma, Psychology, Worry
April 2nd, 2017 by Janine

Music: Jump Around by House of Pain, Got Moves Like Jagger by Maroon 5, Funky Town Gangsta’s Paradise by Coolio, Gin and Juice by Snoop Dogg, Whatta Man by Salt’N’ Pepa (1994!!!). Many many great tracks from the past, particularly hip hop played at the end of the ski/sightseeing day, on the way down in the gondola, via JWL’s phone and with her knowing all the lyrics – seriously impressive or an affliction as she calls it!
Medical Update:
No Chemo, No Hospital this week – yee ha!
Infection: No
Temp: Normal
Mental Health – Nourished by great friends, awesome views, fresh mountain air and being away on a holiday with my hubby (our first, over 5 day, non-New Zealand holiday since 2009, much needed).
WARNING:
I do not advocate travelling abroad during induction chemo treatment. A body’s immune system is weakened during chemo and there is a higher risk of infection. However, in my case, there were extenuating circumstances so a trip to Canada was my idea of the perfect accompaniment to my treatment plan!
Missing Out or A Dream Realised?
Standing on top of a mountain at Banff and Lake Louise had been a dream of mine for many, many years. I had the good fortune to go to Vancouver, Whistler and Blackcomb in 2003 and absolutely loved the experience; the only thing missing at the time was my new lover Mr H, who I had left behind in London. So, as soon as was possible, we planned another trip.
In 2009, a great bunch of old and new friends gathered from all over the world in Meribel, France for a week of skiing. We had a blast. We’d always talked about doing a repeat; State side or in Canada. I had planned it once before in 2012/13 and then cancelled. It was an awful time; I felt like I had really let friends down. We were almost ready to book and then for responsible financial reasons we pulled the plug.
That was not going to happen again. So, we waited until we had the funds, then contacted S & J to see if they were keen on joining us in Banff and Lake Louise. They said yes. We set a date. Easy. We put out the ‘all points invitation’ to the 09 ski bunnies and P & G took the bait – they were in! Fabulous! Regretful “can’t come this time” messages flowed from the rest of the peeps; we quickly knew the score. 6 of us, perfect. We booked. We started getting excited. This was my big post doctorate reward. Sure, it was expensive but it was worth it. I even booked premier economy flights on the return for a bit more comfort for our weary post ski bodies. I couldn’t wait.
Then Myeloma struck. Would I have to cancel again? I yelled in my head “I WILL NOT let everyone down again. That is just not me; that’s not how I roll”. Then more quietly to myself, “Ok so let’s get real, girl; you may have to”. One consultant was silent when I explained about our trip of a lifetime and asked, “was there any way we could make treatment work around it please?” I promised not to ski. I stated, “it would be such good mental health” and “It would give me time to catch up and process everything that’s happened since January”. The other consultant was “yes, we can work with that” and pointed out my trip was timed for the non-chemo week of cycle one; “just be back to start cycle two on the 3rd April”. YAY!
THANK YOU, Universe.
Precautions
The main mission was to make sure I didn’t get any colds or infections right before or while I was away. Dr L wrote me a fantastic letter for obtaining travel insurance which pointed out that I currently did not have any complications and wasn’t go to die on anyone in the next 12 months (take note British Airways and Canada Customs). By the way my extenuating circumstances are that I’m young, fit and healthy with no kidney or otherwise damage despite having Myeloma. If the opposite was true, I think travel abroad would have been foolhardy, and unfair to the clinical team trying to help me get better.
Made It!

After eight hours of wearing double masks (my ears were a bit sore by the end of the flight) and tight leg compressors to prevent deep vein thrombosis, being grilled by Canadian customs who reacted to my mask, and three times interwove asking me when we were leaving into the conversation (presumably to check I wasn’t coming in to their country to seek treatment), I made it to Canada with Simon.

Being on top of the world, breathing in the air, the views, the company– it was like nothing else. I even coped with not skiing though it looked amazing; good base, snow overnight most nights, gorgeous sunny and high sky days and the slopes were not busy at all compared to European pistes! Oh well, next time. Bring on remission.

“Caribou, Caribou” was the cry from J. “Look out of your window!”. Si and I raced to our balcony and watched four Caribou saunter down Fox street before turning into Cougar Street. (I love the street names in Banff; Muskrat St, Bear St, Squirrel St, Antelope Lane, Lynx St, Wolf St..). The guys grabbed cameras and went to capture the perfect pic.
They were a beautiful sight and one that couldn’t have been organised better by a Banff tourist board. We discovered later that they were not Caribou at all, but Elk! (Hence the title for this post). They did not seem phased by human beings being on their patch. Fabulous to see. We wondered what other sights we could rack up while being here and hoped for Moose, Wolf and Bear!

The six of us piled into HMS Sasquatch (our nickname for the monster of a vehicle we hired) and headed up to the slopes, went sightseeing to Lake Louise and Two Jack Lake, and took on liquid refreshment at the fabulous Fairmont and Post Hotels. It was like living in a fairy tale or Narnia, snow covered trees, beautiful light, photo opportunities in every direction.



P (obsessed with bears) gave us the report. Apparently just up the road, grizzly number 122 (aka the Boss) had woken from hibernation early. Given last year he munched his way through two other bears and a sheep on waking – I decided to stay well away from him! P on the other hand seemed keen to race to the last known sighting spot!

Tears and Mindful Thoughts
Tears one morning. They’re close to the surface and hit me when I’m least expecting them. They tend to come when someone says something lovely or is particularly kind. This day was a bit different; “I don’t want to die” flashed up, very quickly and passed, but it was there. It was a bit of a shock though gone in a moment. A thought passing through. Like all other thoughts. Coming and going. To be observed. A thought not worthy of attention, of being ‘bought into’, unless it was a thought that served me. I let this thought go. I took a deep breath. Mindful. Grateful.
No Regrets
Everywhere we went in Canada we were met with friendly, helpful people who adore being in the mountains (including a lot of Kiwis and Aussies, many of whom were on their second season). The service was great. Every café had gluten free menus and were more than willing to help meet diet needs.
My decision to travel felt reinforced and validated at every step and no more so than when sitting in the outdoor hot pool at Banff’s Fairmont Palliser spa looking at mountains in all directions, drinking in the fresh air and being pampered to the hilt. I am so glad I went and didn’t do what I would have done in the past; think “I had better ‘be good’, ‘do the right thing’ and if the standard medical guidance is not to go abroad, then ‘I shouldn’t go abroad’.
Knowing I may have a short and finite time on this earth helps with decision making and helps discard some old ways of being and thinking. It has made me check in with whether I am spending my days in the way I wish to spend them and notice who gets to have a say in that. Going to Canada was one of the best decisions I have ever made for my own mental health; taking all the precautions possible to keep myself well, while away, was the necessary and balancing price to pay for that decision. No regrets.
Psychology
Mental health and mental strength comes in many different forms. Yes, it can be about being stoic, practical and positive in times of crisis. It can also be about taking time to examine what it is we need, in and of this moment, and to consider honestly, what is stopping us from having that need met; a fear, a lack of voice, a habit in the way we think or have always behaved, in similar situations?
It doesn’t matter what we have thought or done in the past; we can always choose to think and behave differently now. Isn’t that what learning life’s lessons is all about? Learn, then do something differently and therefore experience a different result.
Cognitive Behavioural Therapy (CBT) examines links between and cycles of; thoughts, feelings, behaviours and physical sensations. It helps us understand whether the cycles are helpful and serve us well or are unhelpful and no longer serve us, our values, healthy function or goals. CBT strategies such as challenging our thoughts in a constructive, non-judgemental way, help to weaken and break the links between unhelpful thoughts and behaviours. Ultimately this leaves space to create supportive, useful links between thoughts and behaviours. These usually result in more manageable or desirable feelings and better physical sensations.
In this case, I looked at the links between my thoughts about ‘doing the right thing’, how that made me feel (constrained, resentful, mixed with good), my resulting behaviour (to do something I didn’t really want to do or forgo something I had planned for myself i.e. not travel) and the physical sensations (tense). I gently challenged this cycle and the assumptions that underpinned it such as ‘there is only one way’ and ‘you must always go with the first option medical teams advise’.
I thought about what I needed (to go to Canada as planned), weighed up the risks (my otherwise good health with the risk of getting an infection) and I decided I could manage and minimise the likelihood of getting an infection by; caring for myself well, not letting myself get cold, taking all precautions such as double masks when on the plane and in public areas, and not skiing.
I then chose to think and behave differently from the constraints I have applied in the past. While I would normally do things by the book when others in authoritative positions are involved, I decided, this time, that I knew what was best for me, negotiated it with the medical team and reaped the benefits. If I had cancelled and stayed home, I know I would felt disappointment, anger, resentment, bitterness at the Myeloma and sorry for myself.
This way I didn’t experience any of those unwanted, negative feelings.
Instead, I felt intense happiness, empowered and ALIVE, ON TOP OF A MOUNTAIN!

Acknowledgements:
Images and Content: The Fun and Fabulous Ski Bunny Travel Companions; S & J, P & G, & Si.
Illustration (Grizzly): Sapphire Weerakone
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Psychology for Cancer Tagged with: Cancer, CBT, Chemotherapy, Cognitive Behavioural Therapy, Mental Health, Myeloma, Psychology, Travel
March 23rd, 2017 by Janine

Music: Fat Boy Slim – Where You Iz (Where you is, is where it’s at, and you can’t beat that with a baseball bat); Far L’amore (awesome dance track from the film The Great Beauty), VCMG Spock.
Medical Update:
Full dose Chemo plus new drug by intravenous Zometa (bone builder)
Follow up e-Coli urine test – all clear
Ferritin (iron) levels improved from slight anaemic to within normal range
| Test |
High/Low/Normal |
Right Direction? |
| Total Protein |
79 N |
YES! |
| Albumin |
35 N |
|
| Kappa Light Chain |
|
|
| Lamba Light Chain |
|
|
| Urea |
5.7 N |
|
| Calcium |
2.20 N |
|
| White Cells |
2.59 L |
No, as expected (AE) |
| Haemoglobin (Hb.) |
111 L |
No, AE |
| Platelets |
243 N |
|
| Neutrophils |
1.11 L |
See-sawing AE |

Pin Cushion
Day one this week went pretty smoothly. S came and kept me company and we talked about her trip to Norway over the weekend. By 5pm I was very tired and my back around my weak T7 area (mid back) was sore though not hugely so. My slightly swollen ankles, dry eyes with eyelids sticking to the eyeballs didn’t phase me; eye drops and putting my feet up for a while helped with those. The coconut water added to my water bottles during and post chemo also seemed to prevent the headaches of last week. So, all good.
Day two was a slightly different prospect and once again I needed to find my voice. I’d been awake at 1am, 2.30am, and 3am before eventually getting up at 4.10am. The lack of sleep and waking up soaked through probably reduced my patience and tolerance level for the whole day. The rest of the day had started well; raced up for early blood test at 7.30, raced to get the lovely K to work his magic on my hair (why not have perfect hair for the last day of chemo on your first cycle!) and managed to get back on time for noon and my chemo appointment. Then the fun and games began.
A nurse I hadn’t worked with before tried to put in the cannula. She had trouble finding a vein and I know that can happen as Chemo goes on though I was somewhat sceptical at this stage. My arm and hands were warm so cold wasn’t the culprit. I thought about asking Nurse L to come and do it but thought I should give this new Nurse a go. She was sweet yet apologetic for everything and seemed slightly clumsy. A bad day? After two goes of pushing a needle into me only for it to be a bit painful and no vein was found, I asked if Nurse L could do it. To her credit the first Nurse apologised again and explained it was policy for exactly that to happen, that after two attempts to insert a cannula a different Nurse is asked to try. Interesting, that had not happened last week with another Nurse, G, who had rooted around until he found a vein on the third attempt. I would not let that happen again.
Nurse L came over and using the back of my arm got the cannula in first time, pain free. Got to love that woman. Next, when the original Nurse came to change one of the intravenous bags over, the cannula-to-bag connection broke (this had never happened before). Once again to her credit she apologised and explained saying the line may still have worked but to be safe she had replaced the whole line (fortunately the cannula could stay in place). I made a note to ask for Nurse L, Amy or M next time.
Blood
How often do you look at your poo or the paper you wipe your bum with? Who has time? Well I seem to be doing this a bit more, fortunately or unfortunately depending on your point of view. This week at about 5pm on day two, I spotted blood, quite a lot of bright blood on the paper and then in my stool. This concerned me, I so didn’t want to have an infection that would stop me doing this trip of a lifetime to Canada. I decided to see if it stuck around or went away. My temperature was fine so I didn’t panic immediately.
Evening snooze and Steroids were working their magic so I was still awake most of the night and eventually went to bed at 4.30am. Got up at 8am. Temperature was still fine but blood was still there. Felt cold and shivery flu like muscle ache symptoms but I’d been warned this might happen thanks to the Zometa so no panic there and felt better by 10am. Finally called the on-call Haematology Registrar at Kings and they suggested a watch and wait approach too so all fine. The blood had stoped after another day.
That may be because my body had bigger fish to fry; like killing cancer and hey maybe some nasty cancer cells went out with the blood. Now that was a nice thought. Ha, here you go nasties – ejected from Janine’s body forthwith, never to return, thank you! Die. Die. Die. I started singing my little ditty; “I’m killing cancer cells and saying sorry to the good cells that have to go with them”. It always cheers me up though I’m getting sick of the Nashville twang version. Might try rapping it next.
Extra supplies and tips for travel
Because my immunity is lower than usual I had been emailing and speaking to Dr L about how to look after myself while travelling and away. He sorted a prescription with some back up alternative antibiotics in case I got an infection and suggested I got loperamide in case of diarrhoea, paracetamol and also plasters to cover any small wounds. Sorted.
We also talked about masks. He explained that wearing a mask was very considerate of me regarding others though wouldn’t help me much. When someone sneezes or coughs and shares germs, it’s the tiny molecules at the end of the spray that get everyone and they are small enough to pass through a mask. I said I’d double up the masks. Dr L laughed and said “I’d rather you could breath!”. He did make some suggestions about how to adjust the aircon on the plane if I did find myself unable to move away from a germy splutterer which were helpful. He insisted the main thing was that I didn’t get cold, or pick up a cold or virus and he emphasised that I would be more vulnerable to this happening as the Chemo worked its way around my immune system. I tried to reassure him that I would take every precaution possible.
We said goodbye to S. It was time. Her hubby was missing her badly and his birthday was imminent. It was so good to have her here and she helped make the first month of Chemo bearable. Thank you Universe for aligning her visit with my need for extra special bestie help and support. Thank you S for making the longer stay happen. D, thanks for sharing her!
Psychology – Asking for Help
Asking for help is a strength. It is not a weakness. Asking for help does not mean you are weak or needy or less than; it means you are human. People need help to achieve big goals in life. The tennis player doesn’t reach his local team champs or the final of Wimbledon without the support of the person who had taught him/her to play tennis in the first place or the person who continues to help him/her play week in and week out, now; a coach, a tennis racquet stringer, an opponent. Many, many people help contribute to one person’s goals in life.
When you have a difficulty, big or small, asking for help is a powerful message and gift for others as well as for yourself. It lets people know they can contribute to you and that it is also OK for them to ask for help when they need it. You will not burden them; you can ask for help in a very specific way, with clarity about what you need and in a way that leaves them informed and free to choose. If they experience a feeling of burden, that is not your concern, it is their experience, and one they would need to manage by finding their boundaries and voicing them (in the same way you could if you had said yes to helping someone).
If you are open and honest with the people you are asking for help from, and clear about how you would like them to help, then it is up to them to manage themselves if they say yes to helping. So ask for help, especially if you are going through a complex health challenge like Cancer. You can ask friends, neighbours, family, medical professionals, your GP; ask to be referred to a psychologist, nutritionist, physiotherapist if you feel that would help you meet a need.
I have asked a friend to stay longer, to carry my urine, to research nutrition. I have asked my husband to help me to speak to my parents about the best time for them to visit and asked him to help me stick to who I want to be through this stage of the Cancer process. I have asked my consultant to answer seven questions at the beginning of each week of Chemo. I have asked the MacmIllan team for help getting referrals to learn about financial entitlements, access to massage and for a place to sleep between tests. I have asked friends to leave any sadness at the door. I have asked neighbours for referrals to a nutrition therapist and to take in parcels of books and food. I have asked my consultant for a referral to a psychologist and a dietician. I have asked friends to meet, to not meet, to forgive me if I’m not quick to respond to emails.
I HAVE ASKED FOR HELP. HELP has been forthcoming from every angle. People often want to help and you can make it easy for them by letting them know what help you need. My asking has not been met with annoyance or judgement but with thanks and love. If you ask people to help in ways that you know play to their strengths then you make it even easier for people to help you though don’t let that stop you either, just ask. If they can’t help or don’t know how to help in the way you are requesting, it is up to them to say No or suggest an alternative way of helping that may meet your need and match what they can offer.
The right people around you, at the right time, with the right help for you and your needs, can be a significant and positive part of the healing process, so why should you miss out on that?


Acknowledgements
Images: Stephanie Kemp and Nurse L
Posted in Chemotherapy for Myeloma, Psychology for Cancer, Symptoms and Side Effects Tagged with: Asking for help, Cancer, Cannula, Chemotherapy, Myeloma, Psychology, Zometa