April 19th, 2017 by Janine
My veins are not playing ball. According to one Nurse they are spidery, superficial and collapse as soon as a needle comes near them. This is the accumulation effect of the Carfilzomib drug and not unexpected. I had hoped this side-effect may take a bit longer to kick in but hey I want the drug to work so I will take some of the after effects! For each needle insertion attempt that fails – is it Bad Karma? Maybe for my veering off course with my plans… the odd coffee, sip of alcohol, not enough rest…a fabulous slice of chocolate fudge cake on hubby’s birthday (hey I’m only human!).
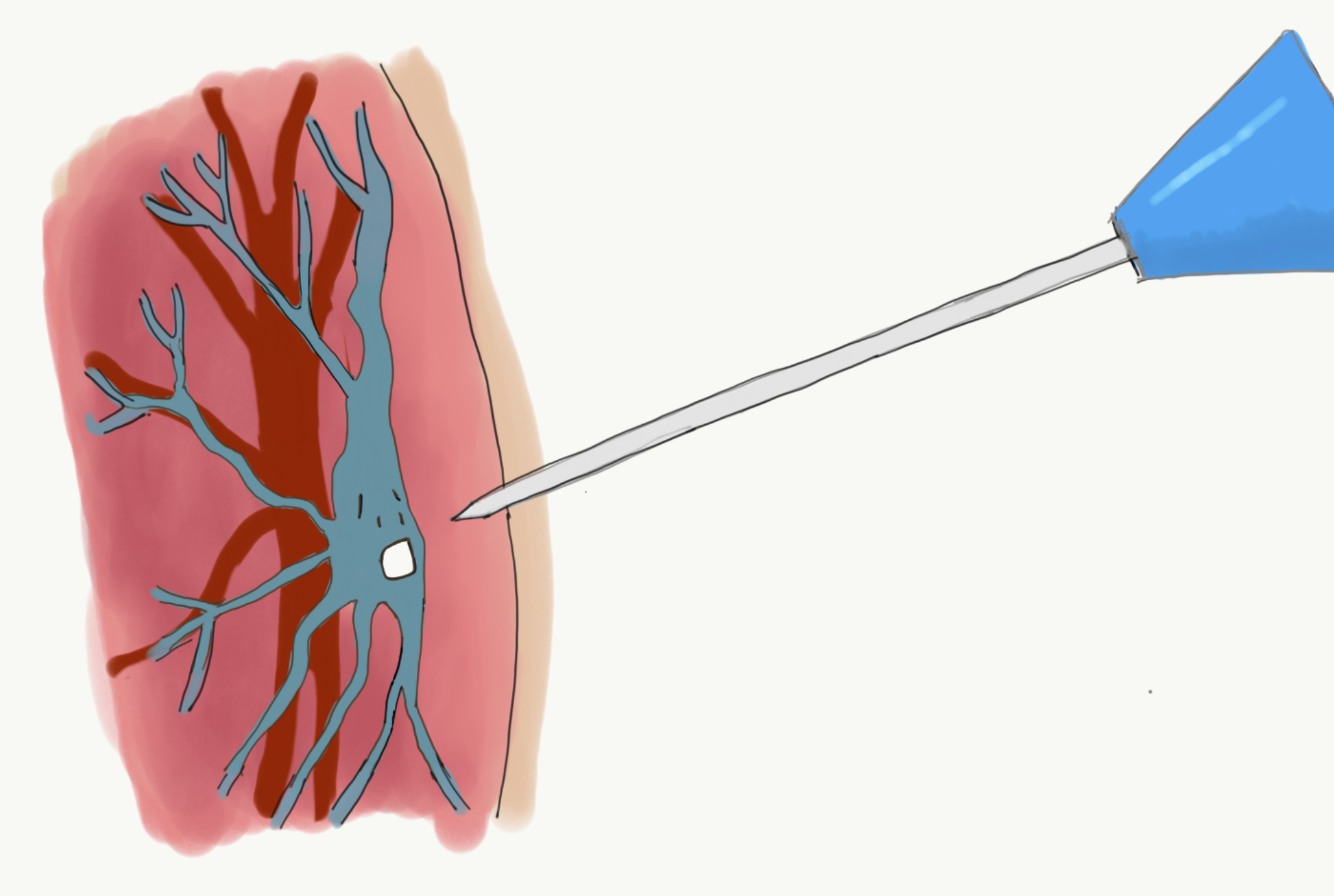
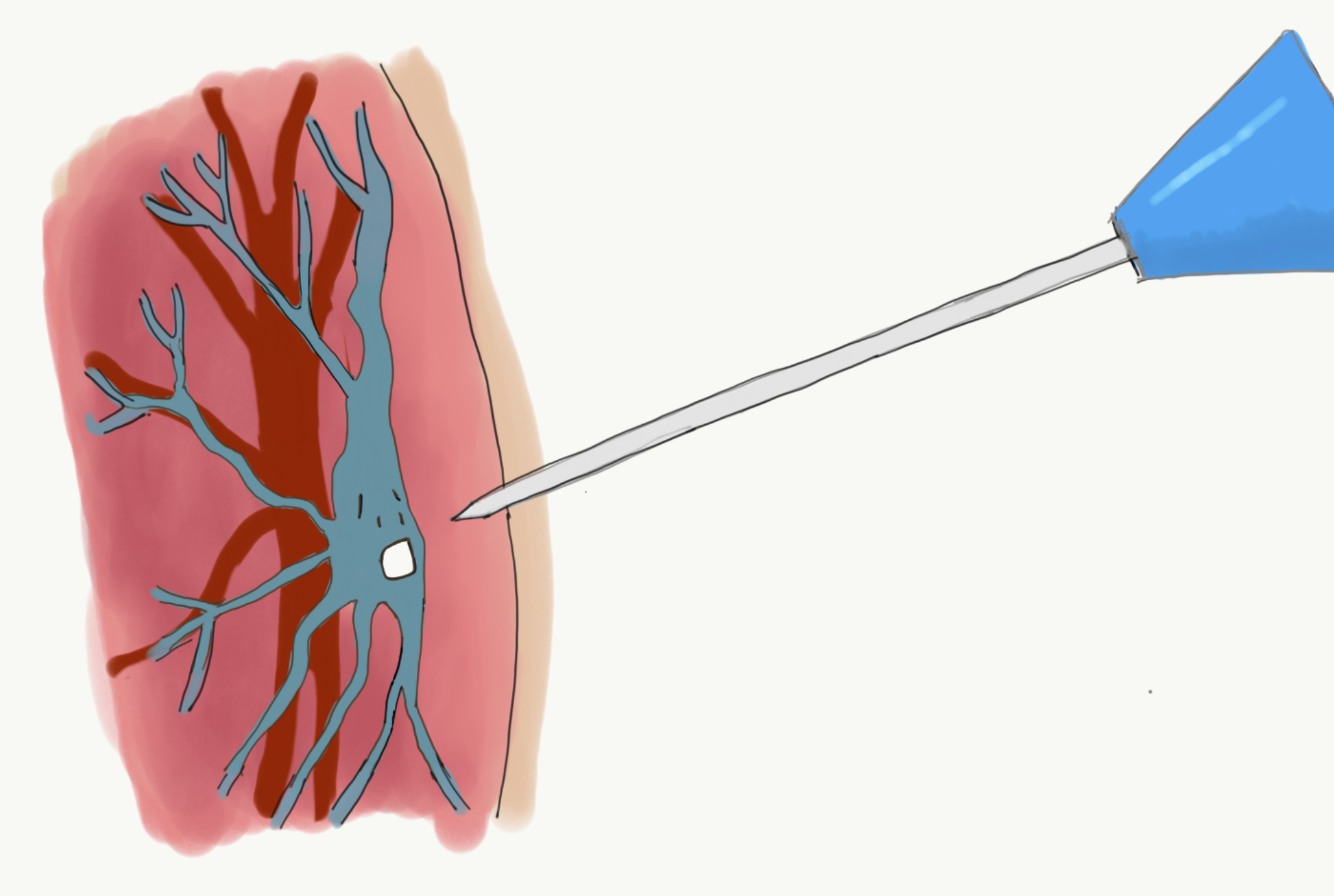
On the first day of my veins playing ‘hide and seek’ (Nurse L’s description) and after two Nurses had taken two to three pin cushion moments on my arms (with my permission) they called in K. As he and Simon bantered about K being the ‘big gun’ and having a ‘big probe’, I discovered what K had brought with him was an ultrasound machine, and that he is one of the few (possibly only) Nurse trained on the Chemo day unit) in using ultrasound for finding veins. In that moment, I loved K; he found a vein quickly and had the cannula in my arm in a flash. The hours of trying to find a vein were not in vain!!
So yesterday when Nurse L said, ‘I’ve come to make friends with your veins’ I said ‘absolutely’ thinking that just because it been hard to find them last week didn’t mean it had to be hard again this week. Unfortunately, that was not the case and the ever-cautious Nurse L was wonderful and genuinely sorry it wasn’t going smoothly. My next request was, could we not muck around any further today please, and get K and his ultrasound. This is when I found out K wasn’t in. K of course is allowed a day off (or two!) however I was unimpressed that only one person can use the machine I need. I imagined that given they know of the accumulation effect of Chemo, I am not the first person to have elusive veins.
Nurse G said he was rusty on using the ultrasound but he’d give it a go. He showed me the images of my veins disappearing as soon as a gentle pressure from the probe was applied in my arm. He abandoned it and said he wasn’t confident enough to use it successfully. Good news though; he checked the back of my left arm and said he could see a vein. He checked whether it be ok to try otherwise they would probably have to insert a PICC line. I didn’t want a PICC line before absolutely necessary so I gave the go ahead, hoping like hell it would work. I could have kissed him, straight in, a little sore but the needle didn’t escape the vein; Si and I escaped the Chemo unit by 5pm.
Kicking in to rationale mode, I started thinking;
- It’s not my fault I need an ultrasound, or that only one Nurse seems to be able to do it; I will always need that Nurse to be available on my Chemo days
- The scenario above is not the Chemo Unit Nurses fault
- It is an unacceptable scenario
- I shouldn’t have to have a PICC line earlier than necessary just because it’s convenient for staff
Moving into problem solving mode; I decided I need to
Ask my consultant;
- How to resolve this; is there another nurse from another team who can be scheduled/ available?
- Can K be scheduled for my Chemo days (cover when he’s on leave)
- How quickly can another Nurse be trained to use ultrasound?
Also ask my consultant about below…
- How much does a private Nurse with right skills cost, can they attend NHS site, can they bring ultrasound machine or use NHS equipment (liability, insurance, clinical trial, other
PICC lines are peripherally inserted central catheters (long, flexible tubes) that are put into a large vein above the bend in the elbow, threaded into a vein until the tip sits in a large vein just above the heart. PICC lines can make things easier for Nurses and for me; it means there is always a line into a vein (with a removable cap) that enables a bag of intravenous drugs to be easily attached; there would no longer be a need to poke around with needles to put a cannula in or to take blood.

On the flip side, PICC lines stay in, require a local anaesthetic and chest X-ray (to check positioning) which are no big deal but are more procedures, and insertion may need to be done multiple times to get the right position. PICC lines get in the way of clothing, need cleaning and re-dressing weekly (Mondays would become even busier visits to hospital), the lines stay in for weeks or months, non-Chemo weeks would then involve visits to hospital. Finally, they are another daily reminder that I have cancer and how my life is different now. I knew i would happily have one when it’s necessary; it just doesn’t feel necessary yet when ultrasound searching for veins has worked.
Today was also a case in point for deferring PICC for as long as possible. I kept my arm and hand warm all morning, under two thermals and a glove. Nurse L found a vein first time. Lovely.
I was in and out of hospital in under two hours.
A tough week ended in A GOOD DAY!
Acknowledgements:
Co-Content: Hubby.
Image: Macmillan information sheet on PICC Lines
Illustration (Scaredy Vein): Sapphire Weerakone
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma Tagged with: Cancer, Cannula, Myeloma, Needles, PICC Line, Ultrasound
April 9th, 2017 by Janine
A cracking question
A cracking question and one that had crossed my mind when I first started learning about Myeloma. Most of us have heard of Leukemia, or know someone who has requested donations for a fun run they are doing in the name of a charity, supporting people living with Leukemia or sponsoring Leukemia research. It seems Myeloma and Lymphoma are less visible or talked about. To rectify this, please find a wee overview of their similarities and differences below.
Do keep your questions coming.
They are helpful to me and I am sure they may be helpful to others too. It is fine to ask; What is X?, How are you coping with Y? or Are you afraid of Z? All questions make me think, reflect and ensure I am staying informed and open with myself, and others, about all aspects of this journey. So seriously, even though you have heard it a million times before: No question is a silly question!
Differences and Similarities
Multiple myeloma and myeloid leukemia have much in common. The names are similar, because they are both cancers that start in the bone marrow. Many of the symptoms are similar, and even some of the same drugs are used to treat both diseases. However, they are two distinctly different entities. Multiple myeloma and myeloid leukemia involve different cell types; B plasma cells and myeloid line of cells respectively.
Lymphoma specifically affects the lymph nodes. The type of lymphoma is based on the origins of the cancer cells. Some start in the lymphatic system (Hodgkin’s), while others begin in the white blood cells (non-Hodgkin lymphomas).
Differences
| Topic |
Leukemia |
Multiple Myeloma |
Lymphoma |
| Stats (UK, 2014):
New Cases
Deaths
Survival (10+yrs, 2011)
Preventable Cases |
9534
4584
46%
15%
|
5501
2928
33%
<1% |
2106 (H) 13605 (n-H)
355 (H) 4801 (n-H)
80% (H) 63% (n-H)
45% (H) 6% (n-H) |
| Cell type |
Myeloid |
Type B Plasma |
|
| Arises in |
Bone Marrow and Blood in form of Myeloblasts and Lymphoblasts |
Myelium
(Bone marrow) |
Lymphatic system, or white blood cells |
| Some Symptoms |
|
Bone Fractures |
|
|
Risk Factors associated with an increased chance of developing the disease
|
· Pre-existing blood disorders eg. MDS or MPN
· Age – most forms of leukaemia are more common in older people. The main exception to this is ALL in which peak incidence is in children
|
· Age—Most myeloma patients are between 50 and 70 years old
· Race— Almost twice as common in Black populations as it is in White and Asian populations
|
For Hodgkin’s;
· Infection with infectious mononucleosis
· Age—Hodgkin’s disease occurs most often in people between ages 15 and 34, and in people over the age of 55
· Epstein-Barr virus may increase a person’s risk of Hodgkin’s disease
· Acquired immune deficiency syndrome (AIDS)
For Non-Hodgkin’s;
· Unprotected exposure to strong sunlight
· A high-fat, low-fibre diet
· Smoking or the use of tobacco products
· Excessive alcohol consumption
· Organ transplantation
· Infections with human immunodeficiency virus (HIV) or human T-cell leukemia/lymphoma virus (HTLV-1)
· Infections with malaria
· A history of infectious mononucleosis (caused by an infection with the Epstein-Barr virus)
· Helicobacter pylori (H. pylori) bacterium, which has been identified as a cause of stomach ulcers
|
Similarities
| Topic |
Leukemia |
Multiple Myeloma |
Lymphoma |
| Blood cancer |
X |
X |
X |
| Scientists unsure why one person is more likely than another to get this cancer |
X |
X |
X |
| Exact causes unknown |
X |
X |
X |
| Starts in bone marrow |
X |
X |
|
| Some Symptoms (e.g. anaemia, bruising and infections) |
X |
X |
|
| Drug treatment (some) |
X |
X |
|
| Risk factors associated with an increased chance of developing the disease |
· Exposure to high levels of radiation and particular chemicals, especially benzene and some chemotherapy drugs
· Particular genetic disorders e.g. Down’s syndrome
· Gender— more common in men than in women
|
· Exposure to certain workplace chemicals and large amounts of radiation
· Gender— more common in men than in women
· A family history of myeloma
|
For Non-Hodgkin’s;
· Environmental factors such as radiation, chemicals, and infections
· Genetic disease of the immune system
· Gender—more common in men than in women
· Family history of lymphoma, particularly brothers and sisters
|
Leukemia (also spelled Leukaemia)
Leukemia is cancer of the blood cells, usually affecting the white blood cells, which causes these cells to not work properly.
There are four main types of leukemia; acute myelogenous leukemia (AML), chronic myelogenous leukemia (CML), acute lymphocytic leukemia (ALL), or chronic lymphocytic leukemia (CLL). In addition to these, there are other types and subtypes of leukemia.
Leukemia can occur in either the lymphoid or myeloid white blood cells. Cancer that develops in the lymphoid cells is called lymphocytic leukemia. Cancer that develops in the myeloid cells is called myelogenous leukemia. The disease can be either acute (begins abruptly and is usually short lived) or chronic (persists for a long period of time).
Acute leukemia involves new or immature cells, called blasts, which remain very immature and cannot perform their functions. The blasts increase in number rapidly, and the disease progresses quickly. In chronic leukemia, there are some blasts present, but they are more mature and can perform some of their functions. The cells grow more slowly so the disease progresses gradually.
Myeloma
Multiple myeloma is a type of cancer that affects certain white blood cells called plasma cells. Plasma cells are part of the immune system, which helps protect the body from infection and disease. Like all white blood cells, plasma cells begin their development in the bone marrow, the soft, spongy tissue that fills the centre of most bones.
When cancer involves plasma cells, the body keeps producing more and more of these cells. The unneeded plasma cells—all abnormal and exactly alike—are called myeloma cells. Myeloma cells tend to collect in the bone marrow and in the hard, outer part of the bones. Patients with multiple myeloma suffer bone fractures in parts of the bone where the cancer is lodged. Ninety percent of patients have cancer lodged in different bony locations, which is why it is referred to as “multiple.”
In most cases, people who develop multiple myeloma have no clear risk factors. Scientists believe the disease may be the result of several factors (known and/or unknown) acting together. (Wish I knew what they were so I avoid the same combination of factors again!!!)
The name “myeloma” is somewhat deceiving because this cancer does not involve myeloid cells. It gets its name because it arises in the myelium, or bone marrow.
Lymphoma
Lymphoma is a type of cancer that originates in the lymphatic system. There are two main types of lymphoma. Hodgkin’s lymphoma (or Hodgkin’s disease) and non-Hodgkin’s lymphomas.
Hodgkin’s lymphoma or Hodgkin’s disease causes the cells in the lymphatic system to abnormally reproduce, eventually making the body less able to fight infection. All other types of lymphoma are called non-Hodgkin’s lymphomas.
Cancers that spread to lymph nodes from other parts of the body are not lymphomas.
The lymphatic system, the tissues and organs that produce, store, and carry white blood cells that fight infections and other diseases, includes the bone marrow, spleen, thymus, lymph nodes, and lymphatic vessels. It is important for filtering germs and cancer cells from various parts of the body. Lymphoid tissue is found in many places throughout the body, including lymph nodes, the thymus (found behind the chest bone and in front of the heart), the spleen (on the left side of the abdomen next to the stomach), the tonsils and adenoids, in the bone marrow, and scattered within other systems such as the digestive and respiratory systems.
Acknowledgements:
Cancer Research UK
http://www.cancerresearchuk.org/health-professional/cancer-statistics
Sylvester Comprehensive Cancer Centre (University of Miami Health System) http://sylvester.org/cancer/leukemia-lymphoma-and-myeloma/education/definition
Leukaemia Care
http://www.leukaemiacare.org.uk/
Multiple Myeloma Research Foundation MMRF
https://www.themmrf.org/
Livestrong
http://www.livestrong.com/article/215375-what-are-the-differences-between-multiple-myeloma-myeloid-leukemia/
Illustration: Sapphire Weerakone
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Diagnosis, Your Questions Tagged with: Cancer, Differences, Leukemia, Lymphoma, Myeloma, Similarities, Statistics
April 2nd, 2017 by Janine

Music: Jump Around by House of Pain, Got Moves Like Jagger by Maroon 5, Funky Town Gangsta’s Paradise by Coolio, Gin and Juice by Snoop Dogg, Whatta Man by Salt’N’ Pepa (1994!!!). Many many great tracks from the past, particularly hip hop played at the end of the ski/sightseeing day, on the way down in the gondola, via JWL’s phone and with her knowing all the lyrics – seriously impressive or an affliction as she calls it!
Medical Update:
No Chemo, No Hospital this week – yee ha!
Infection: No
Temp: Normal
Mental Health – Nourished by great friends, awesome views, fresh mountain air and being away on a holiday with my hubby (our first, over 5 day, non-New Zealand holiday since 2009, much needed).
WARNING:
I do not advocate travelling abroad during induction chemo treatment. A body’s immune system is weakened during chemo and there is a higher risk of infection. However, in my case, there were extenuating circumstances so a trip to Canada was my idea of the perfect accompaniment to my treatment plan!
Missing Out or A Dream Realised?
Standing on top of a mountain at Banff and Lake Louise had been a dream of mine for many, many years. I had the good fortune to go to Vancouver, Whistler and Blackcomb in 2003 and absolutely loved the experience; the only thing missing at the time was my new lover Mr H, who I had left behind in London. So, as soon as was possible, we planned another trip.
In 2009, a great bunch of old and new friends gathered from all over the world in Meribel, France for a week of skiing. We had a blast. We’d always talked about doing a repeat; State side or in Canada. I had planned it once before in 2012/13 and then cancelled. It was an awful time; I felt like I had really let friends down. We were almost ready to book and then for responsible financial reasons we pulled the plug.
That was not going to happen again. So, we waited until we had the funds, then contacted S & J to see if they were keen on joining us in Banff and Lake Louise. They said yes. We set a date. Easy. We put out the ‘all points invitation’ to the 09 ski bunnies and P & G took the bait – they were in! Fabulous! Regretful “can’t come this time” messages flowed from the rest of the peeps; we quickly knew the score. 6 of us, perfect. We booked. We started getting excited. This was my big post doctorate reward. Sure, it was expensive but it was worth it. I even booked premier economy flights on the return for a bit more comfort for our weary post ski bodies. I couldn’t wait.
Then Myeloma struck. Would I have to cancel again? I yelled in my head “I WILL NOT let everyone down again. That is just not me; that’s not how I roll”. Then more quietly to myself, “Ok so let’s get real, girl; you may have to”. One consultant was silent when I explained about our trip of a lifetime and asked, “was there any way we could make treatment work around it please?” I promised not to ski. I stated, “it would be such good mental health” and “It would give me time to catch up and process everything that’s happened since January”. The other consultant was “yes, we can work with that” and pointed out my trip was timed for the non-chemo week of cycle one; “just be back to start cycle two on the 3rd April”. YAY!
THANK YOU, Universe.
Precautions
The main mission was to make sure I didn’t get any colds or infections right before or while I was away. Dr L wrote me a fantastic letter for obtaining travel insurance which pointed out that I currently did not have any complications and wasn’t go to die on anyone in the next 12 months (take note British Airways and Canada Customs). By the way my extenuating circumstances are that I’m young, fit and healthy with no kidney or otherwise damage despite having Myeloma. If the opposite was true, I think travel abroad would have been foolhardy, and unfair to the clinical team trying to help me get better.
Made It!

After eight hours of wearing double masks (my ears were a bit sore by the end of the flight) and tight leg compressors to prevent deep vein thrombosis, being grilled by Canadian customs who reacted to my mask, and three times interwove asking me when we were leaving into the conversation (presumably to check I wasn’t coming in to their country to seek treatment), I made it to Canada with Simon.

Being on top of the world, breathing in the air, the views, the company– it was like nothing else. I even coped with not skiing though it looked amazing; good base, snow overnight most nights, gorgeous sunny and high sky days and the slopes were not busy at all compared to European pistes! Oh well, next time. Bring on remission.

“Caribou, Caribou” was the cry from J. “Look out of your window!”. Si and I raced to our balcony and watched four Caribou saunter down Fox street before turning into Cougar Street. (I love the street names in Banff; Muskrat St, Bear St, Squirrel St, Antelope Lane, Lynx St, Wolf St..). The guys grabbed cameras and went to capture the perfect pic.
They were a beautiful sight and one that couldn’t have been organised better by a Banff tourist board. We discovered later that they were not Caribou at all, but Elk! (Hence the title for this post). They did not seem phased by human beings being on their patch. Fabulous to see. We wondered what other sights we could rack up while being here and hoped for Moose, Wolf and Bear!

The six of us piled into HMS Sasquatch (our nickname for the monster of a vehicle we hired) and headed up to the slopes, went sightseeing to Lake Louise and Two Jack Lake, and took on liquid refreshment at the fabulous Fairmont and Post Hotels. It was like living in a fairy tale or Narnia, snow covered trees, beautiful light, photo opportunities in every direction.



P (obsessed with bears) gave us the report. Apparently just up the road, grizzly number 122 (aka the Boss) had woken from hibernation early. Given last year he munched his way through two other bears and a sheep on waking – I decided to stay well away from him! P on the other hand seemed keen to race to the last known sighting spot!

Tears and Mindful Thoughts
Tears one morning. They’re close to the surface and hit me when I’m least expecting them. They tend to come when someone says something lovely or is particularly kind. This day was a bit different; “I don’t want to die” flashed up, very quickly and passed, but it was there. It was a bit of a shock though gone in a moment. A thought passing through. Like all other thoughts. Coming and going. To be observed. A thought not worthy of attention, of being ‘bought into’, unless it was a thought that served me. I let this thought go. I took a deep breath. Mindful. Grateful.
No Regrets
Everywhere we went in Canada we were met with friendly, helpful people who adore being in the mountains (including a lot of Kiwis and Aussies, many of whom were on their second season). The service was great. Every café had gluten free menus and were more than willing to help meet diet needs.
My decision to travel felt reinforced and validated at every step and no more so than when sitting in the outdoor hot pool at Banff’s Fairmont Palliser spa looking at mountains in all directions, drinking in the fresh air and being pampered to the hilt. I am so glad I went and didn’t do what I would have done in the past; think “I had better ‘be good’, ‘do the right thing’ and if the standard medical guidance is not to go abroad, then ‘I shouldn’t go abroad’.
Knowing I may have a short and finite time on this earth helps with decision making and helps discard some old ways of being and thinking. It has made me check in with whether I am spending my days in the way I wish to spend them and notice who gets to have a say in that. Going to Canada was one of the best decisions I have ever made for my own mental health; taking all the precautions possible to keep myself well, while away, was the necessary and balancing price to pay for that decision. No regrets.
Psychology
Mental health and mental strength comes in many different forms. Yes, it can be about being stoic, practical and positive in times of crisis. It can also be about taking time to examine what it is we need, in and of this moment, and to consider honestly, what is stopping us from having that need met; a fear, a lack of voice, a habit in the way we think or have always behaved, in similar situations?
It doesn’t matter what we have thought or done in the past; we can always choose to think and behave differently now. Isn’t that what learning life’s lessons is all about? Learn, then do something differently and therefore experience a different result.
Cognitive Behavioural Therapy (CBT) examines links between and cycles of; thoughts, feelings, behaviours and physical sensations. It helps us understand whether the cycles are helpful and serve us well or are unhelpful and no longer serve us, our values, healthy function or goals. CBT strategies such as challenging our thoughts in a constructive, non-judgemental way, help to weaken and break the links between unhelpful thoughts and behaviours. Ultimately this leaves space to create supportive, useful links between thoughts and behaviours. These usually result in more manageable or desirable feelings and better physical sensations.
In this case, I looked at the links between my thoughts about ‘doing the right thing’, how that made me feel (constrained, resentful, mixed with good), my resulting behaviour (to do something I didn’t really want to do or forgo something I had planned for myself i.e. not travel) and the physical sensations (tense). I gently challenged this cycle and the assumptions that underpinned it such as ‘there is only one way’ and ‘you must always go with the first option medical teams advise’.
I thought about what I needed (to go to Canada as planned), weighed up the risks (my otherwise good health with the risk of getting an infection) and I decided I could manage and minimise the likelihood of getting an infection by; caring for myself well, not letting myself get cold, taking all precautions such as double masks when on the plane and in public areas, and not skiing.
I then chose to think and behave differently from the constraints I have applied in the past. While I would normally do things by the book when others in authoritative positions are involved, I decided, this time, that I knew what was best for me, negotiated it with the medical team and reaped the benefits. If I had cancelled and stayed home, I know I would felt disappointment, anger, resentment, bitterness at the Myeloma and sorry for myself.
This way I didn’t experience any of those unwanted, negative feelings.
Instead, I felt intense happiness, empowered and ALIVE, ON TOP OF A MOUNTAIN!

Acknowledgements:
Images and Content: The Fun and Fabulous Ski Bunny Travel Companions; S & J, P & G, & Si.
Illustration (Grizzly): Sapphire Weerakone
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Psychology for Cancer Tagged with: Cancer, CBT, Chemotherapy, Cognitive Behavioural Therapy, Mental Health, Myeloma, Psychology, Travel
March 23rd, 2017 by Janine

Music: Fat Boy Slim – Where You Iz (Where you is, is where it’s at, and you can’t beat that with a baseball bat); Far L’amore (awesome dance track from the film The Great Beauty), VCMG Spock.
Medical Update:
Full dose Chemo plus new drug by intravenous Zometa (bone builder)
Follow up e-Coli urine test – all clear
Ferritin (iron) levels improved from slight anaemic to within normal range
| Test |
High/Low/Normal |
Right Direction? |
| Total Protein |
79 N |
YES! |
| Albumin |
35 N |
|
| Kappa Light Chain |
|
|
| Lamba Light Chain |
|
|
| Urea |
5.7 N |
|
| Calcium |
2.20 N |
|
| White Cells |
2.59 L |
No, as expected (AE) |
| Haemoglobin (Hb.) |
111 L |
No, AE |
| Platelets |
243 N |
|
| Neutrophils |
1.11 L |
See-sawing AE |

Pin Cushion
Day one this week went pretty smoothly. S came and kept me company and we talked about her trip to Norway over the weekend. By 5pm I was very tired and my back around my weak T7 area (mid back) was sore though not hugely so. My slightly swollen ankles, dry eyes with eyelids sticking to the eyeballs didn’t phase me; eye drops and putting my feet up for a while helped with those. The coconut water added to my water bottles during and post chemo also seemed to prevent the headaches of last week. So, all good.
Day two was a slightly different prospect and once again I needed to find my voice. I’d been awake at 1am, 2.30am, and 3am before eventually getting up at 4.10am. The lack of sleep and waking up soaked through probably reduced my patience and tolerance level for the whole day. The rest of the day had started well; raced up for early blood test at 7.30, raced to get the lovely K to work his magic on my hair (why not have perfect hair for the last day of chemo on your first cycle!) and managed to get back on time for noon and my chemo appointment. Then the fun and games began.
A nurse I hadn’t worked with before tried to put in the cannula. She had trouble finding a vein and I know that can happen as Chemo goes on though I was somewhat sceptical at this stage. My arm and hands were warm so cold wasn’t the culprit. I thought about asking Nurse L to come and do it but thought I should give this new Nurse a go. She was sweet yet apologetic for everything and seemed slightly clumsy. A bad day? After two goes of pushing a needle into me only for it to be a bit painful and no vein was found, I asked if Nurse L could do it. To her credit the first Nurse apologised again and explained it was policy for exactly that to happen, that after two attempts to insert a cannula a different Nurse is asked to try. Interesting, that had not happened last week with another Nurse, G, who had rooted around until he found a vein on the third attempt. I would not let that happen again.
Nurse L came over and using the back of my arm got the cannula in first time, pain free. Got to love that woman. Next, when the original Nurse came to change one of the intravenous bags over, the cannula-to-bag connection broke (this had never happened before). Once again to her credit she apologised and explained saying the line may still have worked but to be safe she had replaced the whole line (fortunately the cannula could stay in place). I made a note to ask for Nurse L, Amy or M next time.
Blood
How often do you look at your poo or the paper you wipe your bum with? Who has time? Well I seem to be doing this a bit more, fortunately or unfortunately depending on your point of view. This week at about 5pm on day two, I spotted blood, quite a lot of bright blood on the paper and then in my stool. This concerned me, I so didn’t want to have an infection that would stop me doing this trip of a lifetime to Canada. I decided to see if it stuck around or went away. My temperature was fine so I didn’t panic immediately.
Evening snooze and Steroids were working their magic so I was still awake most of the night and eventually went to bed at 4.30am. Got up at 8am. Temperature was still fine but blood was still there. Felt cold and shivery flu like muscle ache symptoms but I’d been warned this might happen thanks to the Zometa so no panic there and felt better by 10am. Finally called the on-call Haematology Registrar at Kings and they suggested a watch and wait approach too so all fine. The blood had stoped after another day.
That may be because my body had bigger fish to fry; like killing cancer and hey maybe some nasty cancer cells went out with the blood. Now that was a nice thought. Ha, here you go nasties – ejected from Janine’s body forthwith, never to return, thank you! Die. Die. Die. I started singing my little ditty; “I’m killing cancer cells and saying sorry to the good cells that have to go with them”. It always cheers me up though I’m getting sick of the Nashville twang version. Might try rapping it next.
Extra supplies and tips for travel
Because my immunity is lower than usual I had been emailing and speaking to Dr L about how to look after myself while travelling and away. He sorted a prescription with some back up alternative antibiotics in case I got an infection and suggested I got loperamide in case of diarrhoea, paracetamol and also plasters to cover any small wounds. Sorted.
We also talked about masks. He explained that wearing a mask was very considerate of me regarding others though wouldn’t help me much. When someone sneezes or coughs and shares germs, it’s the tiny molecules at the end of the spray that get everyone and they are small enough to pass through a mask. I said I’d double up the masks. Dr L laughed and said “I’d rather you could breath!”. He did make some suggestions about how to adjust the aircon on the plane if I did find myself unable to move away from a germy splutterer which were helpful. He insisted the main thing was that I didn’t get cold, or pick up a cold or virus and he emphasised that I would be more vulnerable to this happening as the Chemo worked its way around my immune system. I tried to reassure him that I would take every precaution possible.
We said goodbye to S. It was time. Her hubby was missing her badly and his birthday was imminent. It was so good to have her here and she helped make the first month of Chemo bearable. Thank you Universe for aligning her visit with my need for extra special bestie help and support. Thank you S for making the longer stay happen. D, thanks for sharing her!
Psychology – Asking for Help
Asking for help is a strength. It is not a weakness. Asking for help does not mean you are weak or needy or less than; it means you are human. People need help to achieve big goals in life. The tennis player doesn’t reach his local team champs or the final of Wimbledon without the support of the person who had taught him/her to play tennis in the first place or the person who continues to help him/her play week in and week out, now; a coach, a tennis racquet stringer, an opponent. Many, many people help contribute to one person’s goals in life.
When you have a difficulty, big or small, asking for help is a powerful message and gift for others as well as for yourself. It lets people know they can contribute to you and that it is also OK for them to ask for help when they need it. You will not burden them; you can ask for help in a very specific way, with clarity about what you need and in a way that leaves them informed and free to choose. If they experience a feeling of burden, that is not your concern, it is their experience, and one they would need to manage by finding their boundaries and voicing them (in the same way you could if you had said yes to helping someone).
If you are open and honest with the people you are asking for help from, and clear about how you would like them to help, then it is up to them to manage themselves if they say yes to helping. So ask for help, especially if you are going through a complex health challenge like Cancer. You can ask friends, neighbours, family, medical professionals, your GP; ask to be referred to a psychologist, nutritionist, physiotherapist if you feel that would help you meet a need.
I have asked a friend to stay longer, to carry my urine, to research nutrition. I have asked my husband to help me to speak to my parents about the best time for them to visit and asked him to help me stick to who I want to be through this stage of the Cancer process. I have asked my consultant to answer seven questions at the beginning of each week of Chemo. I have asked the MacmIllan team for help getting referrals to learn about financial entitlements, access to massage and for a place to sleep between tests. I have asked friends to leave any sadness at the door. I have asked neighbours for referrals to a nutrition therapist and to take in parcels of books and food. I have asked my consultant for a referral to a psychologist and a dietician. I have asked friends to meet, to not meet, to forgive me if I’m not quick to respond to emails.
I HAVE ASKED FOR HELP. HELP has been forthcoming from every angle. People often want to help and you can make it easy for them by letting them know what help you need. My asking has not been met with annoyance or judgement but with thanks and love. If you ask people to help in ways that you know play to their strengths then you make it even easier for people to help you though don’t let that stop you either, just ask. If they can’t help or don’t know how to help in the way you are requesting, it is up to them to say No or suggest an alternative way of helping that may meet your need and match what they can offer.
The right people around you, at the right time, with the right help for you and your needs, can be a significant and positive part of the healing process, so why should you miss out on that?


Acknowledgements
Images: Stephanie Kemp and Nurse L
Posted in Chemotherapy for Myeloma, Psychology for Cancer, Symptoms and Side Effects Tagged with: Asking for help, Cancer, Cannula, Chemotherapy, Myeloma, Psychology, Zometa
March 17th, 2017 by Janine

Music: Where is the love (Black eyed peas), Beautiful (Christine Aguilera) Living On a prayer Bon Jovi, Me – I’m killing killing cancer, sorry good cells
Medical Update:
Full dose Chemo started (only half last week)
Glucose test: ‘Brilliant’ according to Dr L; normal=awesome pancreas
Dr L’s comment ‘I’m very happy’ with the way things are going
Blood summary (for normal levels see Chemo Wk 1 post):
| Test |
High/Low/Normal |
Right direction? |
| Total Protein |
93 H |
Same |
| Albumin |
36 N |
Yes, up from Low |
| Kappa light chain |
15.02 N |
Yes |
| Lamba light chain |
4.7 L |
|
| Urea |
5.4 N |
|
| Calcium |
2.21 N |
|
| White Cells |
3.48 L |
No, as expected (AE) |
| Haemoglobin (Hb.) |
118 N |
|
| Platelets |
221 |
|
| Neutrophils |
11.31 H |
|
Rollercoaster
I thought I had it handled: the meds, the new schedule of hospital appointments, new food regime, my admin. I’d written everything down: what to take, when; how to take it (with or without food, with or without gloves, morning, midday, night, once, twice or more times a day), listed things to get done, was recording my temperature twice daily and all experienced symptoms. I thought I was keeping on top of it all. I was feeling clever and calm. I was. Then I wasn’t. I felt angry and then a little stupid. I had missed a key drug.
It was Tuesday morning, I was waiting for my cannula to be inserted. A light bulb moment and then a wee bit of panic; I realised I had not taken cyclophosphamide yesterday. Why didn’t the nurse tell me to take it? Was I meant to take it as soon as my consultant gave the go ahead for Chemo? Yes I think I was, yet the instructions were to bring the drug up to hospital so I had expected the clinical team or nurse to tell me when to take it. Oh what a f**k up. I explained what had happened to the Nurse and she said there is no mention of Cyclophosphamide on her medication chart. Later she mentions there is usually a check box for that kind of thing. How much of a calamity was this? It’s a strict clinical trial protocol isn’t it? What happens If I don’t take the right med on the right day?
Nurse M had given me a table chart mapping out which med needed to be taken each day though it doesn’t account for daily frequency nor all of the supplements I’m having to take as well so I had written out a Janine version. Ha! Obviously I’m not quite as on top of everything after all. I spent the end of Chemo day 4 waiting for my consultant to advise the nurses what happens to me now and if and when I should take Cyclo. Dr L comes by about 4pm: “don’t panic, it’s fine, of all the meds to miss, this one was probably best”. He is such a sweetie and seems to say all the right things.
My heart rate (up to 90 bpm) began to return to normal. Dr L suggested I don’t take Cyclo straight away: “it’ll keep you up all night, take it in the morning if you don’t have an infection, fever or high temperature”. Phew. Not a complete disaster then. We talked about the email he’ll send, about it being ok for me to travel (hmmm, hoped he still trusted me to take the meds on time while I’m away) and he checks again that I WILL be back for the start of cycle two. I reassured him I would be.
I felt awesome on Wednesday; the sun was out drenching the garden, I felt pain free and full of energy. I thought; “This is good! I even feel a bit high”. I wondered what was causing the euphoria. Drugs, no doubt. Relief, probably.
A superb short piece of consulting work through a team I wanted to work with had been offered but the start date was yet to be confirmed. Wednesday ended up being a bonus day as I had thought I would be working. It was a cracker of a day. I sat in the garden with S, ate well, relaxed and revelled in not having to race off to a hospital appointment or have saline, glucose and meds shoved into my arm. However, the next door neighbour’s kitten, T, was driving me bonkers.
Psychology – Behavioural Training
I’m chilled out in the sun then out of the corner of my eye, on the garden wall, a flash of white and then another and then a flash of black and white; two paws and a head. A Kilroy moment. Here comes T. He must be dangling down on the other side of the wall, its so cute and funny. I sigh and laugh simultaneously knowing what is coming. I am trying to complete behavioural training with T as he and our cat, Mason, get on well and race around each others’ gardens but T is like a V8 4WD diesel vehicle (a right guzzler); he’s all paws and stomach, bounding around and eating everything in sight.
We like to leave our back door open when we are around. I was trying to enjoy the sun yet train T to stay in the garden and not go into the house (with our neighbour’s permission). The key to any behavioural training is consistency so I told myself I won’t have to do this forever and he’ll get it eventually. I took a deep breath and for the next two hours felt like a yoyo or space ball; up down, up down, up, in out, in out, chase, hiss, “back away from the cat food T”…eventually, though mostly when I WAS looking, he lay down outside, a foot from the door, making a pathetic though cute meowing sound. It could have been a request for Mase to go out to play though frankly, I suspect it was a master manipulator tugging heart strings saying “come on, you love me really, you don’t really mind if I eat you out of house and home”.


Metaphor for Crisis
The up and down with T seemed to be the metaphor for my rollercoaster week. Next thing I know its 3am, I’m awake with an awful thought. It’s always been in my head that we are flying back on the 2nd but I had better check. Sh*t, sh*t and triple sh*t. Yes we fly on the 2nd but we don’t get back in to London until the midday on the 3rd. This can not be happening. The 3rd is a Chemo day and midday does not allow enough time to get blood tests done, consultant review, pharmacy to make up the drug and to get the chemo done. Now what? I scramble around trying to see if the flight can be changed and sure enough it can – if you have a cool £6000. No I don’t think so. I check the site again; hold on, they are still showing as having economy flights back from Calgary as available, albeit for the full price around £900-1000 (a whole flight price again on top of what we have already paid). While not pleasant, it was an option. Si woke and asked me what was going on. I told him and he said “leave it to me”.
Si rang me later saying they can get us back on the 31st for a change fee. I said I can stomach losing one day of our holiday but two is too much; there must be another way and why can’t we get the flight that is showing on the website. Eventually Si gets it sorted and we fly back a day earlier, arriving in time for Chemo the next day. We pay an extra £300 plus for the change instead of £1000 thank goodness though it is for the privilege of flying back economy instead of the premier economy seats we had pre-paid for. I have my first “this is unfair” melt down. Though with the crisis averted I start feeling normal again. I had not been looking forward to saying to Dr L that I’d stuffed up again.
I’d been chatting away to Dr L by email in the evenings and early hours about various little things that needed sorting (who’d of thought an NHS service would include this?) and he pointed out the importance of getting more sleep. Apparently afternoon naps have been proven to “prolong survival”. With the week’s crises thus far overcome, I finally fell into a deep sleep on the couch in front of a random programme, Forensic Detectives (which I secretly like for watching as you don’t have to concentrate; everything is repeated multiple times and it often sends me to sleep).
I wake up with my clever clear and calm possibility renewed and the thought “I have done 4/6 days of Chemo for this month already”. I also wonder if Chemo is tanning me as my bright red cheeks and chest of the morning now looks tanned. Strange, made note to self to ask Dr L about it.
In the mean time, the work start date was still to be confirmed so it looked like Thursday may be free too. Life didn’t wait just because I have cancer or because I was trying to deal with loads of new information and activities; the house insurance renewal turned up, washing still needed doing, bedsheets needed changing…No further crises thankfully.
P.s. S nicknamed my intravenous drip holder C3PO so I gave him some headwear for his trips to the loo…and it kept my scarf clean while in the loo!



Acknowledgements
Images: Stephanie Kemp and with Nurse Amy’s and T’s parent’s permission
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Psychology for Cancer Tagged with: Behavioural Training, Cancer, Chemotherapy, Crises and Stress, Cyclophosphamide, Missed Medication, Myeloma, Psychology
March 10th, 2017 by Janine

So now you show up. Its 3.30am. I’ve only had three and half hours sleep and now you have woken me. Why now Pain? Where were you before? Where were you when I was meant to have known you, during this stage one of illness that I seemed to have skipped? Are you Myeloma pain or chemo pain? Or universe forbid, something else pain? and sheesh, why butt pain? Is that your sense of humour? If it is, you are not very funny. Especially when my heat pack doesn’t stretch that far!
Though….now that I think about it. Thank you. Thanks for not showing up too much in the past. Yes, I’ve been in and out of physio so much that it had begun to feel like a second home. Friends sitting behind me in lectures were probably sick of my constant fidgeting and neck stretching. Yet in the scheme of things, I haven’t been in much pain at all over the years. I’m grateful for that. You haven’t stopped me doing the things I love. Until now. I love sleep and would like some more please!!!
Interesting that you show up tonight when I’m also fasting for a glucose test in the morning so am probably unable to take anything for the pain. Why is that? Having been so kind in the past, are you now going to make up for it? Will you get worse? Will you always be here? You do like to scare people. Scare me.
Do you fancy some mindfulness? I think you do. I think you need some deep, slow, compassionate and kind breaths, deep into the heart of you so that is what you are going to get. Take care Pain. I suspect you and may have to become firm friends before I send you on your merry way. Know this though. Good friends are soul food. They’re uplifting, inspiring, funny and kind so if you want to hang around for any length of time, you have to join that club. There is no room for draining and negativity here. Come on then. Let’s breath together and see what we can discover about ourselves. You, me and breath. Right here. Right now.
Acknowledgements:
Illustrations: Sapphire Weerakone
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Pain, Psychology for Cancer, Symptoms and Side Effects Tagged with: Breath, Cancer, Compassion, Glucose, Mindfulness, Myeloma, Pain, Psychology
March 9th, 2017 by Janine

Medical Update:
FISH test – Myeloma cytogenetic analysis is an examination of the bone marrow cells to look for chromosome abnormalities. It can be an indicator of likely worse response to treatment and lower life expectancy.
My result: NORMAL (YIPPEEEEEEE!!!)
More low down:
Who knew cancer could be fun? Yes, it’s a whirlwind and it’s also a completely new project. I always love the beginning of a project. It’s the middle bit that’s hardest. Though somehow, I normally always find a way to deliver because non-delivery doesn’t really wash with me. So, I have a new project: Understanding and Managing Multiple Myeloma. I’m certainly not bored, there is so much to learn, do, research and action. Using my brain and academic skills to work out a plan for handling this stuff feels great. As Chemo continues, I add to my knowledge of how the clinical trial team works, how my Chemo works and how to get what I need from the hospital and hospital teams.
One of the questions that several friends have already asked is “how is Multiple Myeloma different from Leukemia?”. Watch this space, I’ll do a separate post on this soon!
It’s been a funny old first week of treatment, especially trying to fill a ginormous container with my urine over a twenty-four-hour period and then, because I am not allowed to carry anything heavy, watching Steff literally ‘take the piss’ up to hospital for me! Good to get rid of that, though urine seems to be a theme for the latter half of the week. I end up having to go to the loo every few minutes and begin to suspect I have a bladder infection. Oh yay. Then when blood turns up in my urine too, I panic and think sh*t ‘this is not the start I wanted’; I said ‘smooth’ Universe please. My first week of chemo is meant to be ‘smooth’!!
Thinking about the blood, I start to wonder if I had overdone the Tumeric. After all, I had gone from barely using the stuff, to shoving it into everything because it is supposedly one of the best things you can do for yourself when fighting cancer. (I’ll do a separate post re Nutrition later). The previous day I’d added Tumeric to a green smoothie, drunk two Tumeric Almond Milk lattes and then had more in a curry. I wasn’t in any pain when peeing, (phew) but the stream of red was rather disconcerting.
Anyway, it turned out Tumeric had nothing to do with it and I had managed to pick up an e-coli bug. Lovely. Not. Under instructions, I double my anti-biotic dose. Still I was strangely relieved that Tumeric wasn’t the culprit. The new Tumeric Almond lattes were meeting my need for a warm hot drink when out and about. I have given up coffee and there are only so many mint teas you can drink before feeling like a herb.
I laughed when I got a Whatsapp message from Dad which was signed off ‘Live’ instead of ‘Love’. Even good old auto text was getting in on this Cancer game. Found myself singing to myself this morning, in a vaguely Nashville twang…”I’m killing cancer cells and saying sorry to the good cells that have to go with them”.
Discovered that two of my drugs are sitting in Lactose, something I’ve avoided for an age because I have been intolerant since a baby. If I drink a glass of milk I end up with instant cold, phlegm and other nasties. I talk to my consultant about alternatives but he’s keen for me to hang in there with them if I can; I resign myself to having a runny nose every day. I do love some of the other drugs, especially the steroids. Waking up with energy is such a novel experience for me.
Waiting to go into my second Chemo session, I send an email to a friend about all the great things to do and places to go in Italy near Naples and the Amalfi coast. Fun reminiscing and good pre-Chemo therapy!
Psychology
I start thinking about the lessons I learnt from when I experienced a road traffic accident (RTA) years earlier (an unlicensed driver drove into me from behind, pinning me from the thigh down under his car while I was on my moped and stopped at a red light). I had rushed back to work far too soon after the accident and worried about everything else except healing. I decided that would not be the case this time. This is the time for self-care, self-compassion, for allowing time to receive treatment and recover from it. This is also the time to ask for help (another thing I did not do during recovery from the RTA).
Who do I want to be through this Cancer journey? How might this change as the journey continues, gets harder? I feel Psyched UP. I don’t feel like a fighter or like I’m in a battle – I don’t really relate to or like those words. I feel accepting, practical yet intolerant of anything other than managing this well and giving my body the best chance to overcome this challenge. I reaffirm I want to be clever, clear and calm through this, for as many days as possible, for as long as I can, because right now that is what feels right.
I pick up the fantastic book Mindfulness for Health: A Practical Guide to Relieving Pain, Reducing Stress and Restoring Wellbeing by Dr. Danny Penman and Vidyamala Burch. I have often used this successfully when working with my own clients. I search for great visualisation and meditation tracks on you tube. I download Headspace, the mindfulness app.
End of week one
A social end to the week. Catch up with lots of lovelies from my psychology programme and receive an amazing goodie bag including a mermaid blanket! I manage to go the gym. Exercise feels good. I feel good, happy; like a 70s hippy on Quaaludes. Then I noticed the bruises and tracks on my arm and laugh. Other gym goers who may have noticed me stretching left right and centre probably think I’m a junkie!

© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Psychology for Cancer Tagged with: Blood, Cancer, Chemotherapy, chromosome, cytogenetic, e-Coli, FISH, Mindfulness, Myeloma, Psychology, Tumeric
March 7th, 2017 by Janine
Format for the update posts:
I plan to stick to a similar format each time for these update posts so you can find your way around easily. The core aim is to let people know how I’m doing as the treatment for Myeloma unfolds, to talk about key medical milestones, challenges experienced and whether it has been a good or tough week overall. Other aims are to let you know what the experiences have been, how they have felt and how I’ve coped (or not) and the stuff I have done and used to keep going.
I’ll start with Music. Music that has popped up over the week or that I’ve sought out to keep me going. This will be followed by the medical update. Then I’ll share the experiences, realities of the week and hopefully throw in a few funnies and highlights from beyond the cancer world. Near the end, I’ll highlight the psychological strategies, techniques and psychoeducation I’ve drawn on to help me look after myself, manage what’s happening to me and helped me endeavour to maintain my resilience and psychological flexibility. I may finish here or follow up on a point made earlier in the post or let you know what’s coming up next. In between these update posts, I may share shorter posts in response to questions I’ve been asked or key events that warrant their own attention.
I hope this approach works for you. All feedback is welcome.
So here goes, Chemo week one…
Music: 90s yeah! Rhythm is a Dancer, Snap: I’ve got the Power, Black Box, Music Sounds Better with You. Strike it Up. I Feel Love for the First Time.
Medical Update:
Week one, day one, up early to hospital for blood tests.
Met the fabulous Dr L and Nurse M.
Everyone happy with my blood test results so given green light to go ahead with Chemo.
Myeloma Presence (Baseline from 17th Feb 17): 17% Plasma Cells, 60-70%infiltration on the trephine (bone marrow test).

Blood summary (for normal levels see picture below):
| Test: |
Value: |
High/Low/Normal: |
Right direction? |
| Paraprotein (Abnormal one) |
91 |
High |
|
| Total Protein |
93 |
High |
|
| Albumin |
33 |
Low |
|
| Kappa light chain |
30.3 |
High |
|
| Lambda light chain |
2.29 |
Low |
|
| Urea |
4.4 |
Normal |
|
| Creatinine |
69 |
Normal |
|
| Calcium |
2.23 |
Normal |
|
| White Cell Count |
8.72 |
Normal |
|
| Haemoglobin (Hb.) |
108 |
Low |
|
| Platelets |
238 |
Normal |
|
| Absolute Neutrophil Count |
6.5 |
High |
|


The low down:
Long and smooth day, started at 7.15 and done by 6pm. So relieved when Chemo could go ahead despite my possible bladder infection and need to pee every 15mins! Quite a juggling act. Each time a bag of meds was detached I did a mad dash to the loo so I didn’t have to faff around with taking the drip line with me! I’ll explain how the chemo works another time for anyone who’s interested.
I have never been so understanding about someone’s pubes on a toilet seat before (people going through chemo often lose hair) though do wish they’d read the sign and improvise. That is, wipe with antiseptic after use. Hard to do when no antiseptic wipes were provided and the sign saying to use them is in the wrong place on the back of the door instead of directly ahead of you as you move towards the loo. This was my main bug bear of the day and I will feedback gently. Yet the previous person could have used some soap in loo paper and that would have done the job!
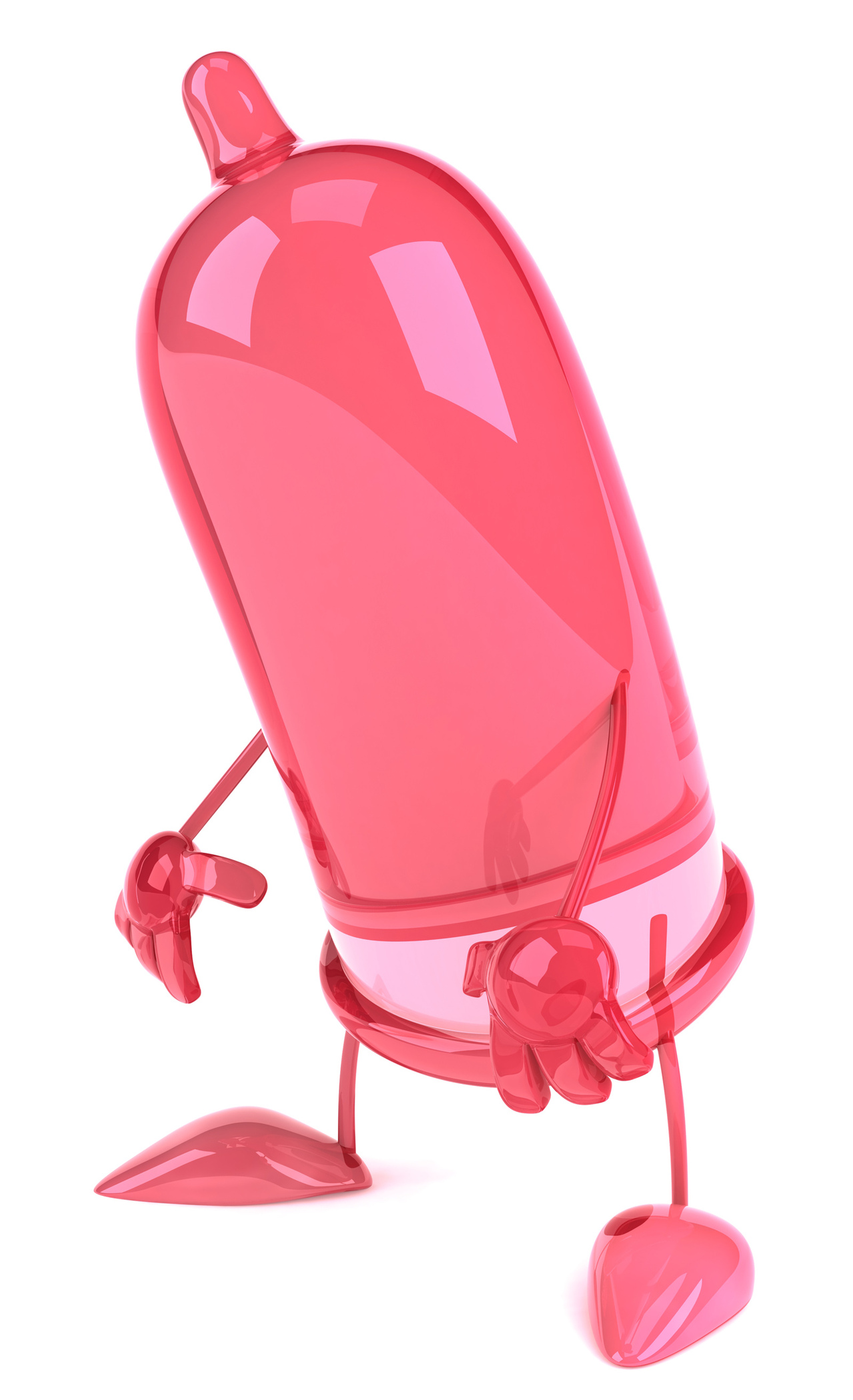
This is turning into a lower bits focus. Felt so good after Chemo, Si and I went down to whoop and holler at our netball team (so hard to not play) and then went out to the pub. Fab people, loads of topics and lots of laughs. We found ourselves sharing our contraception irony…on the trial and when on chemo the last thing the medical team want is for a patient to get pregnant (they’d have to come off the trial, couldn’t get the trial meds wanted, big decisions for patient, birth abnormalities likely). So, even though Si and I have not used contraception since 2007 (!), and have only been pregnant twice very briefly (implant difficulties and a whole other blog needed) we now have to use multiple protection; condoms and a diaphragm with spermicide. Hilarious. Ironic. Oh and the trial team make you sign up to this!
Anyway, the discussion in the pub turned to condoms. The debate was on about who should carry them and when. The males around the table were a firm “NO”, guys should never carry; condoms should always be available at whoever’s place the couple wanting sex end up. I asked “what about spontaneity?” and suggested both parties should carry two condoms. Then F and W pointed out that condoms have inevitably expired and gone manky by the time they are needed and if they are fresh … you wonder how much sex this person is getting?!
Which type to get also sparked a fever: don’t go for those “real life knobbly ones” was the cry – “they’re awful”. Si confessed to being bamboozled by the array of flavours (I thought you’d be so lucky mate!). I laughed about our different purchasing decisions – I’d come home with ‘reals’ and Si had come home with ‘super safe’. Now, he’d never been boring, so I’d clocked that up to him ‘doing the right thing’. The laughs were finally summed up by W saying “yeah, here’s your blog for today, Janine. You should call it Janine on Johnnies; and podcast it!”
Psychology, two points:
- When your energy is good I recommend you take all opportunities to be social; they are good for the soul. You may want to set some boundaries around the social time if you are feeling particularly hyper due to the steroid as I imagine talking quickly, jumping around a lot may be a wee bit draining for friends though highly entertaining! Seriously though, good social support is an immense healer and good friends will get that you are still you and some out of character behaviour is the meds.
- Find your voice. Doctors and nurses are human too. They are wonderfully knowledgeable and yet they don’t know everything (medicine is an ongoing science after all). They don’t know your body and how you and your body are feeling as well as you do.
It is very, totally and always ok to ask any question and share any concerns with medical staff. If they seem irritated or rushed, stay calm, be kind (they are working very hard, over very long hours and doing the best they can; they have bad days too). Then gently insist on their help to get questions answered and concerns aired and heard. Even if they don’t know answers then and there, they may go away and come back with an answer and if they don’t come back, ask the next person. You are the expert in your body and feelings. It is your right to take the best care of your body possible.
If you find it hard to ask, consider asking a wonderfully calm yet confident friend to go with you. Make a list of queries and ask your friend to raise them for you, in front of you so you can hear all answers and ask more if needed. For example, ask if there is an alternative to the drug they have given you, if the drug is in a substance like lactose that you don’t get on with well. There may not be a viable alternative but at least you will know you have done the best thing you could to support yourself or there may be a great alternative and you have just helped your body have one less thing to deal with.
Feel free to ask a nurse why he/she isn’t putting gloves on before he/she puts a cannula in your arm. It’s ok. It’s your arm, your immune system you are trying to help. A good nurse will explain that they may have just washed their hands or go and do it again in front of you or put on the gloves (some nurses wash hands rather than wear gloves before inserting needles so that they have more fingertip control over the needle).
Don’t be afraid to chase up whether a test result is back, ask for copies of all results and make it clear whether you want to know a result now (subject to whether your doctors need you to know). For instance, my Chromosome test was taking ages to come back. I thought it had been lost and I would have to do it again (not fun as this would mean an extra bone marrow biopsy). As the result would not change the first round of treatment (but could have a bearing on prognosis and length of life outcome) I asked staff to make sure the test had come back but not to tell me the result at this stage (unless I needed to know for medical reasons). I did this because I really wanted to sit in ‘everything is going to go really well’ and ‘my first round of treatment is going to be a huge success’. I didn’t want a less than favourable result that I didn’t need to know at this time undermining that thought position. I explained this and the staff understood straight away.
Summary
I recommend you be social when you can (though don’t stay longer than you need if tired) and find your voice with your medical and friendship/family support teams or have a good friend be your voice for you, in front of you.
Ending as I began, talking about ‘lower bits’:
Getting hold of the diaphragm was a whole other saga. My consultant team didn’t know how to get one. The GP had to make a phone call and come back to me. After three hours in the sexual health and family planning clinic, the doc said “we really don’t offer these anymore as there are much more effective and easier forms of contraception”. I said, “I know, I know but I have had to sign up for this”. After hunting through the stock cupboard, she produced a diaphragm. I sighed with relief – at least we can have a sex life now!
Well, thinking about it, sex might be classed as a contact sport, which I’ve been banned from doing! Stuff that! I’m not going the whole time of treatment, the better part of this year, without making love to my husband! Bring on the double barriers!!!

Acknowledgements:
Copy Editor: Stephanie Kemp
Images: Me & Hubby, FreeImages.com
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Psychology for Cancer Tagged with: Cancer, Chemotherapy, Condoms, Contraception, Finding Your Voice, Johnnies, Myeloma, Psychology, Sex, Socialising

February 20th, 2017 by Janine
Most people take more time over choosing a new sofa or hairstyle than I was given to decide on my treatment pathway for Myeloma Cancer. There was no time to waste; my back vertebrae were in danger of fracturing and causing cord compression so treatment needed to start asap. I seal my fate within the week, a time frame Dr R and I could live with. I frantically researched global treatment options versus UK treatment options, NHS versus private care, compared treatment side effects, managed queries in phone calls with Dr R in the evenings, spoke to experts, trawled the internet and discussed pros and cons lists with Hubby.
I had a flash of realisation that no one could make this choice except me. All the other big choices in life recently had been joint decisions; which house to buy, whether to move to Cambridge, when to move back to London, whether we could afford for me to start a business, whether to get a cat, how each clinical psychology course could work for us if I was offered a place. Joint decisions, because they impacted both of us.
Yet, here was the decision that could turn both of our lives completely upside down and I ultimately had to make it alone. A decision impacting my health, my body and what I was going to let someone else do to it. What if I chose the wrong thing and I shortened my life unnecessarily? What if I chose something that turned out to have gruesome side effects for me? What burden was my choice going to cause for Hubby? How long will it be before I am in excruciating pain, breaking bones left, right and centre, paralysed or need full time care?
Pause, breath. I remind myself that survival rates in myeloma are increasing at one of the fastest paces among all cancer types in the UK1. Pause. Breath.
In the end four things kept zooming around my head:
- There is some evidence (though better and more research is needed) that people have better outcomes when they participate in clinical trials2,3.
- Standard care involves Thalidomide. I know it has improved since the old days but the side effects can still be nasty and I just don’t like the sound of it.
- The main trial drug Carfilzomib has had great results for people at relapse stage and it and its side kick Cyclophosphamide have been much better tolerated than Thalidomide.
- I will be monitored like a hawk if I sign up to the trial so reactions and adjustments are likely to be more timely.
- I can always withdraw if I feel the trial is no longer serving me and move to standard care. I don’t want to withdraw yet I can, if I feel it’s necessary.
You guessed it, in the end I chose the trial. It’s called CARDAMON and is being overseen by a partnership between University College London (UCL), Cancer Research UK and Amgen Ltd (Pharmaceutical company). Participant recruitment is taking place at UCL and Kings College Hospital (KCH) and several other UK hospitals.
So, what will be done to my body and its overzealous Myeloma para proteins?
For four months, in one month cycles, I will receive a chemotherapy cocktail of three drugs nicknamed KCD. KCD comprises of:
Carfilzomib (Kyprolis)4,5. This has been used to treat over 4000 myeloma patients world-wide with both relapsed and newly diagnosed myeloma, is licensed for use in the US and approved by the Food and Drug administration (FDA) but is yet to be approved in the UK, hence the trial. It is a proteasome inhibitor that prevents breakdown of abnormal proteins in cancer cells, causing the cells to die. It has only rarely been reported to be linked with the side effect of peripheral neuropathy (pins/needles/numbness in extremities) which can be painful and which has been associated with the drug used in standard care, Velcade (Bortezomib). I will get Carfilzomib by intravenous infusion, through a cannula in my vein on 6 days out of the month. Doesn’t sound so bad…
Cyclophosphamide (Cyclo)6. This drug belongs to a group of drugs called alkylating agents. It works by sticking to one of the cancer cell’s DNA strands. DNA is the genetic code that is in the heart of all animal and plant cells. It controls everything the cell does. The cell cannot then divide into 2 new cells. I will get Cyclo orally by tablets on 3 days out of the month. Doesn’t sound so bad…
Dexamethasone (Dex)7. This is a strong steroid that can suppress inflammation and the immune response, kills cancer cells and usually induces a better response to the other chemotherapy drugs than when chemotherapy is used alone. I will get Dex orally by tablets on 4 days out of the month. Doesn’t sound so bad…
After three weeks in the month of going into hospital every Monday and Tuesday for the above, I get a week off the KCD and don’t have to go to hospital.
I do though have to take a bunch of other meds too, one to protect my kidneys, another to prevent/manage nausea, another to stop a virus outbreak, an antibiotic to prevent infection. These continue during the non-chemo, no-hospital week.
I’ll also start another drug called Zometa8, a biophosphanate with good evidence that it reduces bone loss, fractures and helps to build bones. I will get Zometa by intravenous infusion, through a cannula in my vein on the same day as getting Carfilzomib I think. I’m yet to understand how often this happens.
After four months, my response to the Chemo will be assessed and if my Myeloma para protein level has dropped by 50% or more, the Chemo will be considered a success.
I will then be scheduled for a heavy-duty med to induce stem cell production ahead of stem cell collection.
After recovering from the stem cell harvest, I will then be randomised to either the;
- branch of the trial that receives an autologous stem cell transplant (ASCT; meaning using my own harvested cells) in the same way I would have received one if I had chosen standard care or
- I will go into the branch that receives a further four months of the KCD cocktail
After this, participants in both branches of the trial receive maintenance medication.
So, what is hoped for from all this medication? Short term, the hope is that the standard care response of a minimum of a three-year remission is achieved and for the patients in the continued KCD arm that this remission period is achieved without having to undergo an invasive stem cell transplant. Longer term, the aim is that the treatments, even within the three years of my own remission, will have moved on so quickly (there are already exciting drugs coming down the line in trials) that Myeloma moves from an incurable illness to a chronic illness. A stem cell transplant would then become the final defense at the later stages of the illness.
If this all a lot to take in, I get it. I thought so too and I’m still getting my head around it all. There is a massive new language set that goes with moving in this world of cancer and Myeloma.
Have I done the right thing? I hope so. I feel that I have, with the research and time in which I had to make the decision. Psychological cognitive science theory purports that usually you will choose your choice. It is called choice–supportive bias or post-purchase rationalization9. It is the tendency to retroactively ascribe positive attributes to an option one has selected and it’s a cognitive bias. Therefore, I am highly likely to have a cognitive bias about my decision to choose the trial because not to do so would undermine my choice…and make it much harder to believe the trial treatment will be successful. I usually try to avoid or at least be cognisant to my own biases. In this case, I fully own and embrace my bias about my decision to go with CARDAMON. BRING IT ON!
Acknowledgements and References:
1Myeloma UK. www.myelomauk.org
2 https://academic.oup.com/annonc/article/22/Suppl_7/vii10/214151/How-may-clinical-research-improve-healthcare
3 https://academic.oup.com/annonc/article/22/Suppl_7/vii2/214043/The-impact-of-the-process-of-clinical-research-on
4 CARDAMON Patient Information Sheet; Kings College Hospital; version 4.0; 07Nov16
5 https://www.themmrf.org/multiple-myeloma-knowledge-center/myeloma-drugs-guide/kyprolis/
6 http://www.myelomabeacon.com/resources/2008/10/15/cyclophosphamide/
7 http://www.myelomabeacon.com/resources/2008/10/15/dexamethasone/
8 http://www.myelomabeacon.com/news/2010/06/22/zometa-increases-overall-survival-and-slows-bone-disease-in-multiple-myeloma-patients-asco-2010/
9 http://changingminds.org/explanations/theories/choice-supportive_bias.htm
Copy Editor: Stephanie Kemp
Image: Photo by Angelo Pantazis on Unsplash
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Psychology for Cancer Tagged with: Cancer, Carfilzomib, Chemotherapy, Choice Supportive Bias, Chronic Illness, Clinical Trial, Cognitive Bias, Cyclophosphamide, Dexamethazone, KCD, Myeloma, Para Protein, Post-Purchase Rationalisation, Response to Chemotherapy, Stem Cell Harvest, Stem Cell Transplant, Survival Rates, Treatment, Treatment options, Zometa
February 19th, 2017 by Janine
Informing your parents on your 48th birthday that you have blood and bone cancer is not a common or pleasant thing to do. In fact, it has been the hardest thing to do in this whole journey so far: let family and friends know, see and hear their pain, their sadness, their shock. Sharing my diagnosis and curtailed life expectancy with people whom I love was and is cutting to the bone.
Trying to work out when to tell and who to tell is a challenge too. I had to seek advice from the wonderful J who had recently experienced this dilemma. In the end, Hubby and I agreed we would find out more information first and did as much of that as possible over the 11th to 13th February. Then we planned to tell my parents first, followed by his parents and then my NZ besties who have known me since I was 18 years old: who I knew I could count on to cope (in their different ways), to be hopeful, practical, support me, Hubby and each other.
I realised I needed to tell people quickly as it is quite hard these days with social media and, when you have the fortune to have good friends, who wish to catch up regularly, to get on with your life if you haven’t told them. I anticipated being less available due to Chemo and recovery, fending off ‘how work was going’ related questions and having to explain why my hair was falling out etc. I just thought no shocks should ensue when I rock up to graduation in July, thinner or fatter (from steroids) and sporting new headwear. Anyway, it’s my style to be upfront about what is going on. Well at least I like to think so.
Also, I recognised I needed support: some now (especially humour) and certainly I am likely to need some later during treatment. Hubby needs support too. So, telling people seemed the right thing to do for me (though I do understand why others might prefer to keep it quiet and wait until treatment has taken place).
My parents who live in New Zealand are amazing people, so generous, kind and often overly considerate of others. They are also inspiring, energetic, wise and well educated; great mentors to others. They were firm with me in many ways when I was growing up, yet open and welcomed questions and debate. My parents ensured I had a diverse range of experiences and chances to pursue hobbies; fantastic holidays in NZ, netball, tennis, scuba, plays, ballet, musicals, art and concerts. I remember going to see Rod Stewart when I was 10 and Charley Pride and the Bolshoi. They have wide music interests. My point is, that for so many reasons I am immensely grateful for my parents and my upbringing. I am fortunate enough to have a great relationship with Mum and Dad, one that only keeps getting better. We have always been super independent and have never lived in each other’s pockets, talking once a month or so and trying to meet in recent years at least once a year. It was especially hard to tell them bad news. Especially this bad news.
Mum cried and had to move away from the Skype call. Her natural empathy for others is huge and so close to the surface, I wasn’t surprised at this reaction but it was hard to view. Dad in his usual stoic, practical in a crisis kind of way, hung in there and asked all the right questions. I did my best to be matter of fact, hopeful and clear. I was churning inside seeing the hurt on their faces. We eventually ended the call so Dad could go and look after Mum. Over the next few weeks it took a bit of convincing them not to jump on a plane immediately (imagine me sending shackles for Mum over the ether!) but in the end, they have been amazing as usual, listened to our needs and I am now very much looking forward to their extended visit later in the year. I am very proud of them and how they are coping.
Telling Hubby’s parents was not really any easier except we spoke over the phone so I didn’t see their faces. It all went a bit wrong initially as they were in the car at the time. When we suggested we wait until they were home they insisted on going ahead but then they didn’t know what was coming. When we explained, the call was stopped and started ten minutes later once they were home. I love my parents-in-law (P and T) and Hubby’s Mum. They have all been very supportive. Being visited by P and T the very next weekend was helpful and in the moment I loved T’s assumption that I would beat the odds.
The weird thing and something I really resented was how many people knew I had Myeloma before I was able and ready to tell my loved ones. My dentist and his receptionist knew because I needed his clearance of not needing any dental work before I could start a bone building drug, the beautician at the hotel we stayed in while taking time away to process all the new information and treatment options knew, when I filled out their questionnaire and she gently announced she would not be able to give me the massage I was craving. Scared of a law suit if something went wrong I suspect. She did give me a lovely pedicure and I found myself reassuring and cheering up her and her manager. Looking after others needs about my cancer was something I learned would become a regular occurrence. One I plan to avoid unless necessary and may come to be rude about as I only have so much bandwidth for looking after others’ needs right now. Sounds selfish but true; though working with a couple of private clients still appeals as it wouldn’t be about my stuff.
I laughed as J had warned me in a funny story about her partner who had told ‘everyone’ about her cancer diagnosis when Hubby came home late one night and confessed. He had shared our new challenge with his manager so he could take some time off to attend tests with me. Then ‘he’d spilled the beans’ over a beer and late night commuter trip following hours of standing on a platform and delayed trains; he’d been frustrated he wasn’t home when we had so much going on. I didn’t resent this; he needed to share but it was weird that people I’d never met and had no affiliation with, knew about my stuff before my good friends knew.
Telling my besties was also a logistical timing issue. On one hand, it was fab as S happened to be visiting from the States with her hubby and his daughter. However, it was our birthday week and I really didn’t want to tell her my news before we had been able to celebrate her birthday. This was tough as it felt like I was lying to her and not able to fully connect or spend as much time with her as I had planned to as I raced off to appointments. It was a total relief to let her know and then Skype with my other besties the next morning. As anticipated they were simply wonderful, reeling but managed well and said all the right things. Soon after I sent an email which was a much easier way of communicating my news to my close UK based friends and other special people in my life all around the world. Deep sigh of relief and a wee bit of fear followed. You never know how these things will land.
While telling others has been extremely hard: telling myself about how many years I am likely to live has been strangely easy. I did want a long life but only if it was filled with quality, mobility, activity and intact cognition. This way, with Myeloma, I strangely feel more in control and have a rapidly growing awareness of just how I might want to live life in periods of remission. Instead of living far off in the future my next five years is firmly in focus. Who I wish to spend it with, how I want to spend it, is a close second in my mind behind successfully managing treatment. I envisage kicking this cancer into outer space for as long as possible if not forever. The way I see it, there is no reason why I can’t be one of the first people to experience Myeloma as a chronic illness with long periods of remission over normal life expectancy, rather than have life limited to 8-10 years with frequent periods of hospital visits and new Chemo regimes. That’s what I’m gunning for and requesting of the Universe. So, you see I still want to be special, but I am being much more specific about, how I wish to be special, when speaking to the Universe.

Acknowledgements:
Illustrations: Sapphire Weerakone
Copy Editor: Stephanie Kemp
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Diagnosis Tagged with: Cancer, Chronic Illness, Family, Friends, Myeloma, Sharing bad news, Telling others you have cancer