Category: Myeloma Treatment

February 22nd, 2018 by Janine
Dr L turned to his colleague and said, ‘for someone with Myeloma, Janine’s immune system is a Schwarzenegger’. Hey Arnie, you are now a metaphor for my health status. Who’d have thought?! It sounds so positive and I am very grateful that my precious physical self is coping so well with the toxicity of Chemo. I notice too that I get a little hung up on the ‘for someone with Myeloma’ phrase though more about that in the next post. Now, I want to talk about my relationship with my body. It has become a bit confused.

Can I share a secret? I liked it when cancer, chemo and a diet change caused me to lose weight. I like being closer to 60kg than 70kg. I like how slim and less pear shaped my legs look. I like being size 10 and for a few weeks, size 8. All my life, I have valued being slim, strived for it. I’m not obsessive. I don’t over exercise or starve myself or think about it constantly. Even when I put on two stone from IVF treatment: I hated it but didn’t panic. The weight had context. Once we stopped IVF treatments, I lost a stone quickly and then worked on chipping away at the rest. I like cake. I binge occasionally (or did before this new eating regime). Who doesn’t when there is a pack of dark chocolate hob nobs in the house and the hormones are taking over? I would say I’m weight and health conscious with no extremes.

I’ve never liked my arms: they’re too big. Well, apart from the time I sanded every spindle on a stair case by hand: my arms were toned, like Madonna’s or Geri Halliwell’s. I thought my arms looked great after that. It didn’t last long. Finding tops and elegant shirts to fit my arms has always been a hassle. The welcomed side effect from cancer, chemo and clean eating has been the slightly thinner arms and shirts fitting, for once. I don’t really want to give that up yet…
I find myself struggling. I’m in a tussle inside my head. Too much weight and muscle loss is not healthy, not helpful and goes against Dr L’s advice. He explained that he had noticed that people with Myeloma who keep up with the gym and have some muscle reserve seem to manage the chemo better. I do want to live as long and as well as I can. Yet I find myself loving my new size. I bought a pair of boyfriend jeans a few months into treatment, laughing with a wave of pleasure when I discovered I could fit into a size 10 only to find they slipped off a month later and I’d lost even more weight. Now what do I wear? Nothing in my wardrobe fits!!
At that point, 61kg, it did get a bit worrying. My face was looking drawn. My rib cage and spinal vertebrae were a too visible. I promised Dr L that I wouldn’t let my weight fall further. I expanded my food repertoire slightly (good quality bacon, goats cheese, sourdough toast occasionally) and started the weight training.

Back at the gym, I felt good and waves of relief from feeling stronger. I’d become so weak. I was asking hubby to open jars and water bottles for me and lift anything. This does not fit with my independent and equality philosophy. Yet, I dislike how quickly my leg and arm muscles grow. When my weight started to rise slowly I would find it hard to like what I saw in the mirror. I know it may seem silly in others’ minds. Intellectually, I know I look ‘normal’, ‘healthy’ and would still look heathy even if I did put on weight (I’m fortunate to be tall). Except, somehow it feels like a tug of war in my brain – Janine, don’t put on more bulk, you look good as you are (now size 10-12) versus Janine, you need more muscle and strength to manage Chemo effectively, get yourself to the gym.
For more years than I care to think about, I have gone to buy clothes and come back disillusioned when I have needed that elusive size 13 or 15. It seems crazy to have the same problem at a lower size (now 9 or 11) and with the added complication of my size constantly changing. I can’t afford and wouldn’t want to invest in new sets of clothing every few months yet as my weight goes up and down on chemo, what can I do? Frustrating. I hate being uncomfortable in clothes. I really dislike ill-fitting clothes that don’t help me feel good and enhance how I look in the world. Too loose is as bad as too tight!

Even more annoying, last summer, before diagnosis, I bought some new clothes after ‘making do’ for a few years. Now they are sitting in the wardrobe, barely used as they are far too big. I am in the maintenance phase of treatment, with 3 days rather than six days a month of Chemo and my weight is climbing and fast. I’m 67kg today. Maybe I’ll need those ‘larger’ clothes again in a couple of months. Except, I don’t really want to get any bigger or go back to the size of those clothes again. The 6 days of steroids each month may have something to say about that.
67kg. Nothing to worry about. Yet, I don’t feel good about it. I am beginning to worry that a steroid induced, sharp trajectory up of weight, will set in and hang around for the duration of treatment. There are 16 months to go! That’s a lot of weight gain. That makes me feel sick.
It is also motivating. I’m back on the high veg and protein regime. A few bits of non-clean eating crept in as I celebrated getting through the first 48 (see previous blog) and 9 months of treatment. Then I let the goodies stay, it was Christmas after all. Then I felt sorry for myself with the arrival of two viruses back to back. January came and went, and it’s always the toughest month in UK for me. It’s so often grey, cold, hibernation inducing and all I want to do is eat comfort food!
Oh well, not having the clothes I would like, in the bigger scheme of things, is insignificant really. If I hover around the 65kg mark and I am made of tiny Arnie style muscles, that will be good enough. Viruses and January blues are gone. The revolution is here. February has arrived.
I’m back on track with preventing my body from being a perfect host for cancer. I celebrate a new food focus: FISH. It is easy to do: I am languishing on the beautiful beaches of ANTIGUA for a much-needed holiday. Fresh snapper, mahi and octopus are on the menu. The company is great (hubby and besties), the sun is high, the sea is warm and the forecast is rosy. No time for weight tussles now: The bikini is out and about!
Acknowledgements:
Antigua seascape: Photo by me
Legs and kettle bell: Photo by Maria Fernanda Gonzalez on Unsplash
Clothes hangers: Photo by Christian Fregnan on Unsplash
Shirt and Jeans: Photo by Lyndsey Marie on Unsplash
Muscles: Photo by Alex Boyd on Unsplash
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Finance and Cost, Psychology for Cancer Tagged with: Cancer, Chemotherapy, clothes, muscles, Myeloma, weight
January 10th, 2018 by Janine
Boo!
Did I change career over the last month of 2017, become a lead actor in a thriller? This thing keeps creeping up from behind me, above me, beside me, from below, yelling BOO! It sends my cortisol levels sky high, makes my heart pound and brain race. I’ll be tidying, reading, sitting, walking down the street, thinking about something or standing in a queue, essentially minding my own business, when WHAAAHHH! There it is.
I recognise it straight away. Sometimes, I even feel it sneaking up on me yet it still scares the living daylights out of me. It’s a shape shifter, a dark cloud and an amour piercing arrow. Either way it makes me gasp, scream, crash, sleep, feel defunct. It pulls the ground out from underneath me, leaves me doubting the paths taken and decisions made that previously seemed acutely clear and necessary. It’s an expert protagonist in this production. It doesn’t take direction. It’s a master tease, dangling hope and snatching it away, reminding me, it’s in control. I’m the newbie on set with no Daniel Day Lewis, Dame Maggie Smith or Christian Bale style mentor to guide me. In the meantime, it picks another corner to hide in and I jump through the roof with the next BOO!
It’s not cancer; it’s fatigue.
Fatigue and Fear
Fatigue, is really getting to me. I don’t get enough sleep. I wake every two hours.
I’m also scared. Though I do know I’m alive!
I’m scared of dying young. I’m scared of missing out. I’m scared of making a poor decision; making my condition worse or accelerating its progress. I’m scared of being a burden. I’m scared of not being enough for my husband, of dragging his life down (all the active plans we had). I’m scared he’ll leave me. I’m scared I’ll ask him to leave me, to go off and find someone else, to have a life with more fun, that doesn’t involve or revolve around a wife living with terminal illness. I’m scared that I don’t and won’t again resemble my sense of who I am; an active, full of life, adventurous person who stands on mountains, travels everywhere, is strong, independent, sensual. I’m plain scared.
Fatigue and fear. I feel them. I get paralysed by them. I think about them. And, yep you know it by now (if you have read my earlier blogs)..…
That’s OK. It’s OK that fatigue and fear do that.
It’s natural. I am living with cancer and have had a gazillion sessions of Chemo during 2017, numerous biopsies, scans, endless blood tests, new challenging experiences and learnt a new language of medical intervention. However, just because I face big challenges or can find myself embroiled in fatigue and fear, doesn’t mean I must let these factors take over this whole blog.
I can do a bit of my own shapeshifting, respond rather than react, slowly little by little unlock the paralysis and pull on a cloak of ‘sitting in all the good things’. I can start now. I’m not ignoring fatigue and fear. I’m not denying their existence. I am denying them their take over plans. I am choosing to focus on something else right now.
Today, this blog is going to be about a huge THANK YOU and more Good News!

THANK YOU.
Belated Merry Christmas and / or Happy Holidays and Happy Happy New Year everyone. Thank you ALL, for reading my blog, for subscribing, for commenting, for sharing it with others who may have an interest in the journey, an interest in what has worked for me so far in managing cancer or an interest in the psychology tips and experience I have incorporated.
Thank you too, for all the wonderful cards, calls, skype time, meals together, moments and best wishes my hubby and I have received over the holidays. They are so appreciated. Every single one.
I firmly believe that all your support and encouragement has contributed to my good news. I have felt loved, helped, contained, hopeful and normal at times when things were far from normal. THANK YOU from the bottom, to the top, of my heart.
THE GOOD NEWS.
My December 2017 results are great. In addition to those mentioned in the previous blog, titled 48, my recent pet scan, bone marrow biopsy and MRI have overall been extremely positive. Of the four lesions I was diagnosed with, only ONE near L5 in my lower back took up glucose during the pet scan, indicating active myeloma. Even this lesion took up significantly LESS glucose than it has done in previous scans. Yeah Baby! How good is that?!
I told those tumours they were wasting their time hanging about and I am taking this as evidence that they have been listening and reassessing their landing page! It is wonderful to read the line in the report that said ‘There are no obvious focal uptake abnormalities in the brain’!! Let’s hope no un-obvious ones decide to make an uninvited guest appearance. They’d be about as welcome as a Harvey Weinstein type right now!
There’s more. The bone marrow biopsy did not show any active Myeloma in my blood or bone and, wait for it…my MRI did not show evidence of any new lesion/tumour. Yee Ha!
I do have one caveat; I have some mild degenerative disc disease and loss of height and hydration between vertebrae in my spine; my back is looking a bit older than my years. It is unlikely that I can particularly do anything to repair damage. I can exercise and ensure by back remains strong, doesn’t antagonise the nerves around L5 and otherwise prevents my degeneration from becoming worse unnecessarily. I will check with the physio about what else, if anything, may be possible. It was also wonderful to read ‘the spinal cord returns a normal signal and the brainstem structure is normal’.
Being pragmatic, I am remembering that Myeloma is tricky. It will come back. It can also be a bit lazy and not show up at times in these results. It can take a rest or be working out how to manifest itself in a new way in my blood and bone. HOWEVER, TODAY…
I’m looking on the bright side of life! (How many of you began singing this line? I can’t help myself)
A helpful position to launch from; I start 18 more months of Chemo this week – the maintenance phase on the clinical trial. Let’s see what this brings.
This is infinitely easier to do with wonderful friends, family, readers, well wishes and my so far ‘beyond amazing’, hubby. I appreciate all of you. I really do.

February 2017

December 2017
THANK YOU.
BRING ON 2018.
Acknowledgements
Images; Hands by M & T. Me (February) by Dad. Me (December) by Me. Thank you image by Tumiso @ Creative Commons (free for commercial use, no attribution required);
© 2018 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Psychology for Cancer, Results Tagged with: Biopsy, Cancer, Fatigue, Good News, MRI, Pet Scan, Results, Thank you
December 6th, 2017 by Janine
What a year! I turned 48, I was diagnosed with cancer and I’ve completed 48 chemo sessions. I love the number 48; it seems so symmetrical to me (I love a bit of symmetry). Now ‘48’ has a WHOLE new world of associations!
Warning…I have happy news, and, I’m going to talk about toilet rituals.
First, the rituals.
This may seem very strange to those of you who have always been super careful about hygiene when using public loos. In my defence, I have rarely worried about these things because my childhood in New Zealand was filled with non-traditional toilet arrangements. When you are fortunate enough to spend all day at the beach or walking in the bush or driving long stretches of deserted road or camping in remote sites you tend to get over yourself quite quickly about going to the loo wherever and however.
Doing your business quickly behind a tree, rock, or in a smelly long drop with minimal paper or alternatively leaves or seaweed, is not that unusual. Worrying about being seen was always a bit more bothersome than worrying about bugs, microbes or possible infections! The upshot is; I have never worried about using public loos, ‘catching anything’ or having to use disinfectant. I just focussed on washing my hands well.

Now that my immune system is compromised it’s another story completely….though maybe I’m being a bit anal? (pun intended)
In the Chemo Day Unit, patients are asked to ‘wipe the loo’ with anti-bacterial wipes before and after use. I recently discovered I had developed a wee ritual…Take a wipe, clean toilet seat, fold dirty side in, use clean side to wipe toilet handle, tap, hand wash dispenser, door lock, door handle. Dispose of wipe in bin. Use loo. Wash and dry hands properly – you know the 8-10 step process (depending on the poster). Take new wipe and clean toilet. Goodness knows what bugs I could pick up if I didn’t do this; don’t tell me!
Anyway, this is a new ritual in my life and once again one that seems to consume a little more of my available time and life though hopefully is worth it. It seems so, so far, as I have yet to pick up any major nasties despite lower immunity and chemotherapy for 9 months now. This ritual has now made its way out of the hospital and into public conveniences. AM I being anal? I’ll let you be the judge!


My News
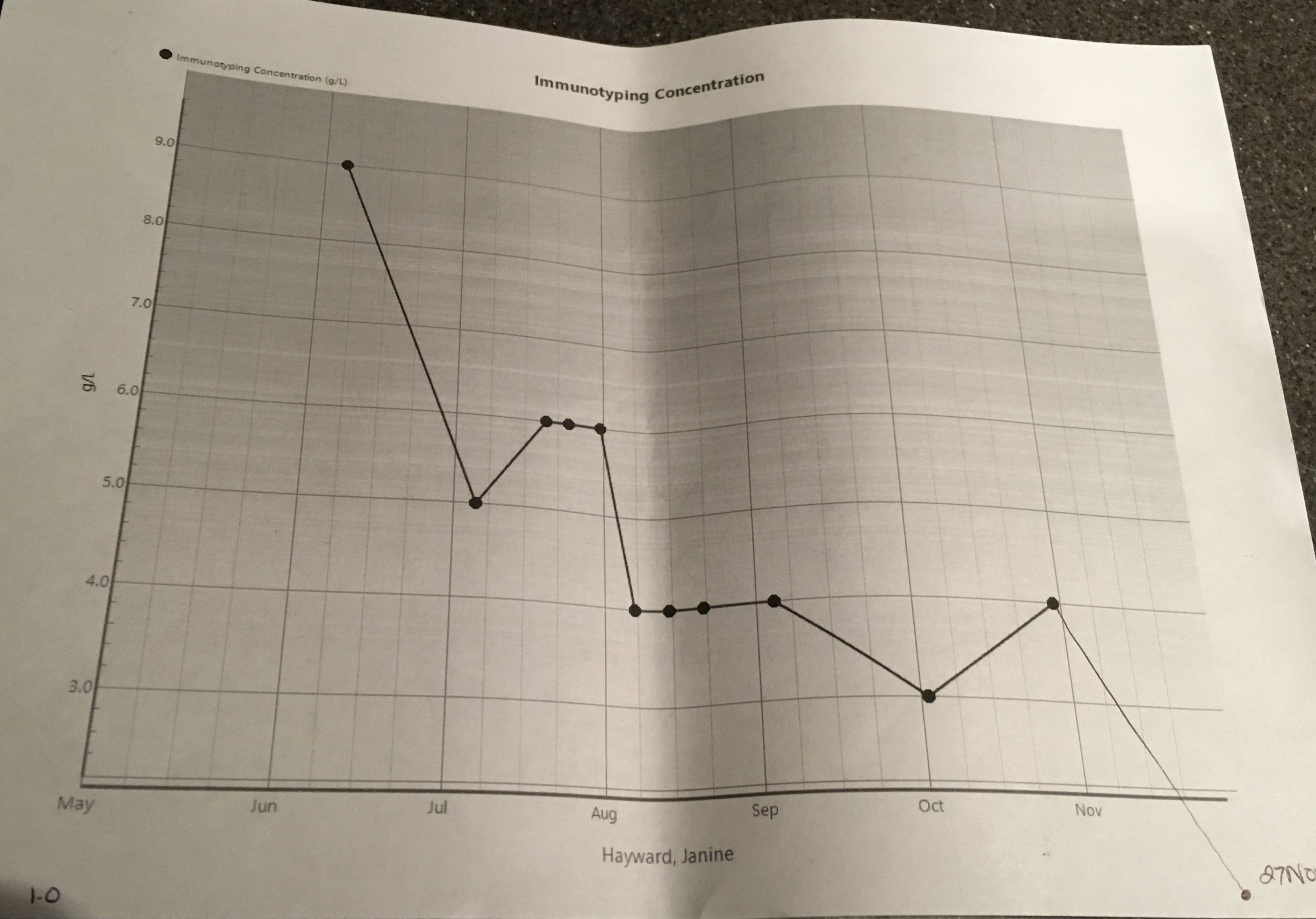
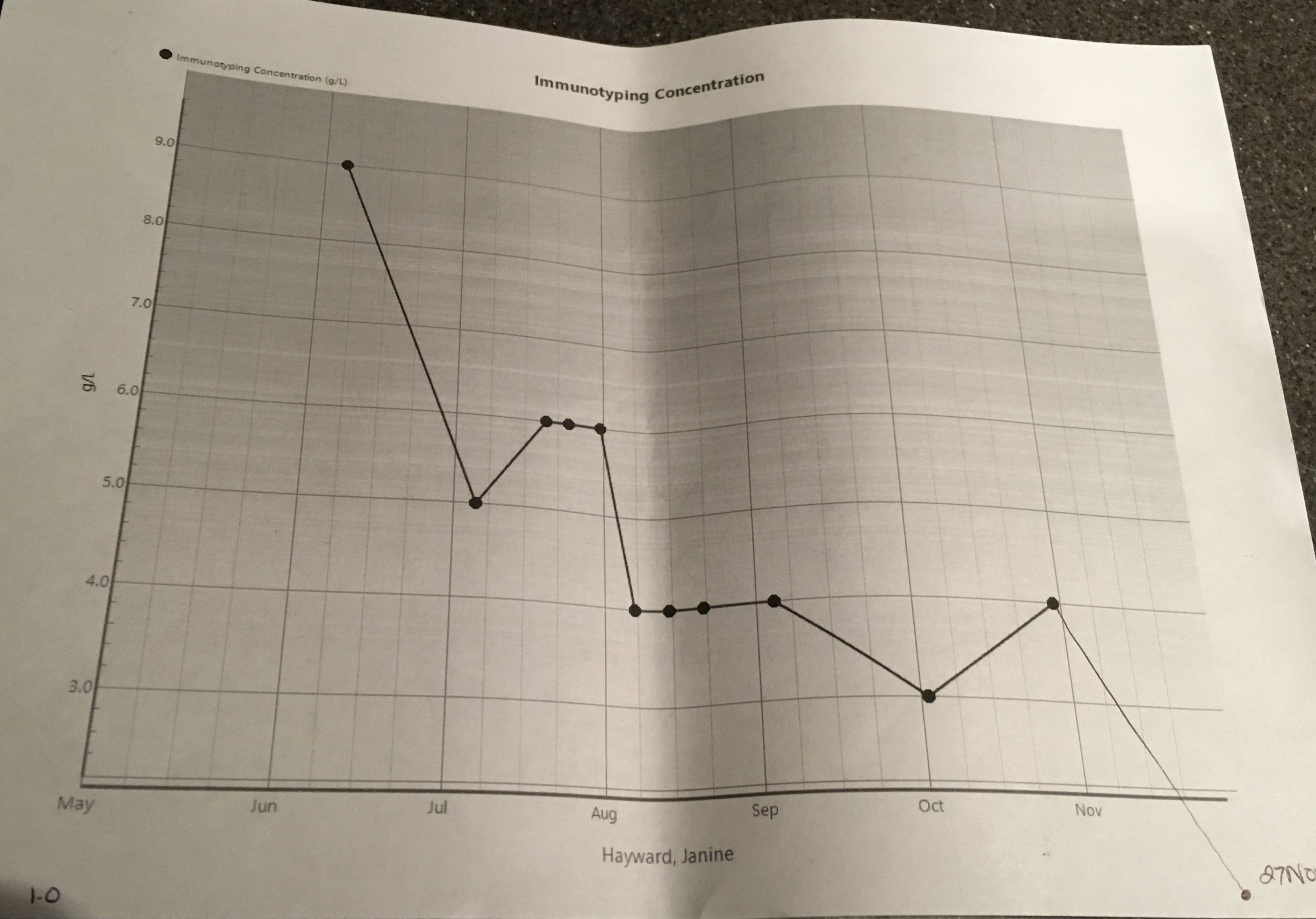
…is happy, positive and hope-FULL…I’m very grateful for it and its effect; a reaffirmation of my faith in my medical team, the drugs and my health and life choices. The Myeloma presence in my body has decreased further in the last few months… It’s down to 1 g/l (42 g/l at its peak) and a may be yet to plateau. Yee ha! Not only that, the serum kappa light chain results are 1.75 mg/l, backing up this great news and described as ‘excellent’ by Dr L. On top of that my liver is doing well. My Hb (Haemoglobin, the protein found in the red blood cells that carries oxygen around) level is back up to 121 g/l so I no longer need to consider taking EPO (yes, the cheaty cyclists’ drug of choice! I’m a tad disappointed. I had wanted to experience how energised I’d feel!) While 121 g/l is lower than the desired normal levels (125 g/l plus) it is great for someone with Myeloma. My kidneys are also doing OK for someone with Myeloma, my Creatinine is 69 umol/L and normal level for women is approx. 45 -90 umol/L (I think; there seems to be some debate!). Lots of good, great news, here. Dr L delivered these details and then reminded me to keep drinking 2-3 litres of water today for kidney care. I imagined my kidneys; bloated, water-logged, bean-shaped balloons, wrapped up in clouds of cotton wool, floating about, relaxed and without a worry in the world.


I’ve had yet another bone marrow biopsy and pet scan (what effect does three doses of radioactive sugar chasing gunk in a year have on one’s body? I guess I’ll find out!). I have an ear numbing full body MRI coming up in a fortnight.
Let’s hope they show (or don’t show lesions at all) that lesions are further dissolved and there are no new uninvited guests!!
What a year.
48.
One number I’ll never forget.
Acknowledgements
Images: Me (graphs va KCH), Long Drop – Sarang (public domain use permission granted)
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Myeloma Treatment, Results Tagged with: Bone Marrow Biopsy, Chemotherapy, Myeloma, Results, Tests, Treatment

October 31st, 2017 by Janine
OK Mr Tumour or more accurately Messrs Tumours. Listen up. Yep, all four of you. You know who you are. You are hanging around unwanted and uninvited. Where do you get off thinking its ok to be dossing about in my body? You’re a greedy bunch, aren’t you? Not contented with one spot, you hunker down in two places in my spine, my shoulder and my sternum. You threaten me with paralysis as you near my spinal cord and grow dark and big. What arrogance! Well, I have some words for you.
I have mindfulness and meditation and you are not going to like them. In fact, I already know you haven’t seen them coming. They have roughed you up a bit with their calm, kind, ease. Aww. Tough. If you can show up unannounced, I sure as hell can unleash mindfulness and meditation on you.
Your resistance is futile. You are already weaker. You can keep trying to hide out, munch on sugars (if I give you any) and try to take over the joint…but I know where you are. Your luck has run out. The Chemo is working. My new diet is working. My NHS medical team is great. I am doing fine. My mindfulness and meditation practice, reminds me this is so. Mindfulness and meditation practice, whether 5 minutes or 35 minutes; it’s getting to you, Mr Tumour (yes you, the large one in my lower spine). I’m talking to you.
YOU are DISSOLVING.
One at a time. Worst, darkest, nastiest first. You are dissolving. I know because I have seen you. My MRI showed me. You are thinner, lighter, dissolving, dying. Don’t feel bad. You are no match for kindness, curiosity, breath, acceptance, listening, powerful visualisation, practice of belief. Belief that my decisions about my treatment have been the right ones for me, that my medical team is the right one for me, the Chemo is the right Chemo for me and that I am doing fine.
My favourite guided meditation reminds me of this.
NOW you are DISSOLVING.
Meditation helps me visualise an all-powerful, protective, transformative, warm, healing light. It wraps up all four of you, Mr Tumour, you and your buddies, letting you know you are not needed. The light heals my body, generates new healthy cells, rids me of you. This same meditation helps me draw energy, power and peace from the Universe, imagine, believe and trust I am in safe hands, doing the best I can do. It is working. You are not running this show or in charge of this gig. I am; with the help and support of mindfulness and meditation.
Mindfulness for sleep. Mindfulness for Cancer. Mindfulness. It helps me to stop. To be. To breathe. To observe. Mindfulness, paying attention, moment to moment, in a kind, curious, non-judgemental way. Not like you, Tumours. You are random, cruel, unnecessary. Yet, thanks to Mindfulness, I accept you. I accept that you are here. I watch you, learn from you, ignore you and listen to you. I accept you have muscled your way in, demanded to be seen, to be heard. With Mindfulness, you don’t get to invade my every moment or even most moments. You don’t get to hurt my sense of who I am. You don’t get to take over. You get to be. Until, you are no longer being.
Listen up Mr Tumour. You are superfluous to requirements. While I accept you are there, I’m just letting you know you can go and take your friends with you. I know you are likely to return in the future; I’m a realist. Right now, you are not needed and not wanted. By the time, you want to make a comeback, I will be stronger than I am now, even more practiced in mindfulness and meditation, and healthier with years of a great low sugar diet behind me. I will have more chemo options and more effective medical solutions at my disposal. I will know more about you, your characteristics and the environment you need to thrive. I won’t provide it. You’ll have to find somewhere else to go or better yet not bother at all. I am ready now. I will be ready in the future.
I might have dark days and dark weeks through this journey Mr Tumour but that is nothing on how uncomfortable I am making things for you. I am not going to fight you. I’m not in a battle. I simply will not be providing the terrain that you want. I see you. You are dissolving. Soon I won’t see you. You are getter weaker. Myeloma may remain but you Mr Tumour are no match for my healing light. You do not have to stick around. Mindfulness and meditation, they’ll remind me why you came and what you can teach me. I won’t forget you. I don’t however, need you. I will watch you dissolve. You can leave now. Thank you.
Three of my favourites;
Meditation
Survive Thrive and “Dawning of the Day” by Aine Minogue
https://youtu.be/MNaqEKtc4Uk?list=PL2a9c2CFCJdlYehE9jochHrjWFMq4AHiu
Mindfulness
https://www.headspace.com
http://franticworld.com/resources/free-meditations-from-mindfulness-for-health/
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Psychology for Cancer Tagged with: Cancer, Dissolve, meditation, Mindfulness, Myeloma, Nutrition, spine, Tumour
August 22nd, 2017 by Janine

Hooked up
My blood spurts everywhere like a regular Fright Night or Halloween movie. The nurse is trying to put a cannula into each arm, a bloody big cannula, much bigger than my normal (ha ha) Chemo cannula. The nurse is new to this treatment and seriously nervous. Great. I’m not in the mood today. The mood. The mood where I am happy to be part of someone else’s learning curve. I’m just not. Now she’s made a mistake and there is blood everywhere. My blood. My very, very, precious blood.
Another nurse pounces with a clamp and gets everything back under control. For now. Except, I feel sticky. My leggings and legs are spattered with blood. The pillows and bed coverings are no longer pristine white. Stressed, I blurt out, ‘I don’t want to be anyone’s experiment’. The nervous nurse (NN, my nickname for her) looks horrified. She reassures me that I am nobody’s experiment. Her body language and voice sound like she is trying to convince herself that everything is OK. I think ‘I can’t afford to lose any more blood; get me someone who has done this A LOT’. But I don’t say this out loud. I hope it, instead. I calm down a bit and give NN, a smile of, ‘it’s ok’. It’s not OK but I figure I need her to be calm. Everyone makes mistakes. In the grand scheme of Myeloma treatment, this wasn’t a bad one (so long as I don’t end up needing that runaway blood).
I am in the Apheresis unit, finally all wired up (ready for ‘take off’?) to a clever centrifuge machine (very CSI) labelled 3OJO (MOJO with a 3? A machine with 3 times the MOJO?). Anyway, this machine specialises in taking blood out of one arm (Vampire-esq), separating out plasma and stem cells and then giving what remains of my blood, back to me, through the other arm (Angel-like). Genius! my niece would say.
I try to relax. The machine’s sound reminds hubby of ‘‘beedie beedie’ so we nickname it, Twiki, and completely ignore the OJO’s in the end. Do you remember the TV show called Buck Rodgers? Twiki is a silver robot (cute but with unfortunate haircut) known in the show for saying ‘beedie beedie’ to everything. Very effective. I’ll think I’ll use it.

Twiki with a lot of mojo (Stem Cell Collection machine)

All the fancy stuff Twiki monitors
I’m quite intrigued by my blood and its component parts…hanging in a bag next to me is the plasma, a funny yellow colour and next to it, slowly, salmon pink (apparently, that’s a good colour) stem cells appear. Also on the line in bags are saline (isn’t it always?) and an anti-coagulant. My lips begin to tingle strangely and I feel a bit faint. I let the nurses know. They have warned me this can happen. My calcium level is ramped up and I’m lowered down a bit in the bed. A song pops in to my head…Blood, Blood, Glorious Blood…There’s nothing quite like it…My Glorious Blood.
Boredom kicks in for hubby soon after arrival, I’m not very talkative today. I can’t sleep because to help collection along I am required to pump the stress ball, all day, only taking breaks for a few minutes every 10-15 minutes. Hubby checks out all the bells, whistles and knobs on Twiki and marginally resists touching them (knobs after all) and is now entertaining himself by dancing on the spot. I’m trying to work out which music he’s listening to because he occasionally is singing out loud, unintentionally I think, and boy his lyrics are dubious! The nurses and I catch a look and laugh. Glad he’s got a day job! Though I’ve secretly always loved his dance moves. I still can’t work out which songs he is listening too. Turns out he’s immersed himself in 70s and 80s and he’s running through Hall and Oates hits (would never have guessed). We share headphones and have a laugh with the past. Today is turning into a retro day.
I arrived at 8.30am and it’s now 5pm and I too, am very bored; so ready to be out of here. I’m waiting for lab results to come back and say they’ve taken enough stem cells. For the last four days, I’ve had G-CSF injections that stimulate the stem cells to move out of my bone marrow and into my blood so Twiki can collect them. This is preferential to the other option of having them collected directly from the marrow (painful, long, more chance of complications, I suspect).
The injections have some seriously weird side effects; they cause pain from inside my bones (ironically similarly to the way Myeloma does…there are so many ironies with this overall treatment process, seemingly making things worse in order to make things better!). At random points, shots of pain would pulse from my rib cage or my pelvis, take my breath away and stop me in my tracks. It would usually be gone within 5-10 minutes and then be back again 10 minutes later or half an hour later or whenever it decided!
Lab results this morning told me the injections had ‘done their thang’ and the detectable level of stem cells in my blood (CD34+ test) was well over the count required to go ahead with Twiki’s collection manoeuvres. Thank goodness. The collection target is 7 million stem cells per kilogram of body weight and I hope it can be done in one hit, today. The results come back and they are good but I still need to rock back up tomorrow (and take another injection). They have collected 5 million. A few more are needed. Hubby and I walk home slowly. I feel shattered.
I’m baaackk! The next morning is a funny affair, no more escaping blood and instead a new approach. Yesterday’s senior nurse seemed to be cautious in approach, going slowly and setting things up so blood clotting was avoided. Today’s senior nurse explains she prefers to deal with problems when they arise and ‘we’re going to go for it’ and monitor everything carefully. Funny, I thought coming in two days in a row for the same treatment would ‘be the same’; a standardised process. I hadn’t factored in the human element and the nurses’ different strategies. Today’s target is 3 million stem cells per kg of body weight so info is plugged into Twiki and I lie back and ?? think of England? More like think ‘please please collect everything needed quickly’. It’s an all-day affair again. My potassium and calcium levels need propping up so I go home with extra meds to add to my ever-growing list.
The call comes through an hour later; they’ve collected another 5 million. Excellent that’s 10 million stem cells altogether. They’re sent off for cryopreservation (storage in liquid nitrogen at some crazy temperature, −196°C). I’m relieved. Maybe that’s enough for three transplants in the future. Maybe I’ll live longer thanks to these. If that’s the case then this last week has been a tiny investment; completely worthwhile.
Turns out from discussions with my clinician later that three transplants are not routinely given at the moment and there is no evidence supporting their benefit. Instead, the transplant team would usually spilt the 10 million stem cells gathered into two larger lots, for each of the two transplants. Supposedly there have been some benefits found for higher amounts of stem cells being used per transplant.
Oh well, you never know. By the time, I need the second one maybe they won’t need as many cells after all and I can eek out another transplant. Or my transplants will be so successful I won’t need a third one. Or it will be what it will be, completely in line with current evidence and practice. I’ll worry about that when it happens.
As part of the clinical trial I am on, I’ve been randomised to another four months of chemo (Carfilzomib, Cyclosphamide and Dexamethazone, half the Dex dose than in the previous four months) rather than an immediate transplant. I don’t need to worry about the transplant details right now unless something goes a bit wrong and the Myeloma comes back with a vengeance sooner rather than later (after all it is always going to come back). I crash for two days (the cat loves it) and feel really shattered for the week.

Post collection rest
The good news about my Myeloma is that its presence in my body after the first four months of Chemo has dropped; the IgG kappa paraprotein level is down to 6g/l after being as high as 42g/l. It’s not quite the 100% response rate I was hoping for but it is damn good. It is not usual for this rate to rise again for a year. I’ll have regular tests and jump on it if it decides to buck the trend.
I’m a bit low in mood and I think this is mainly due to low potassium and not knowing what the next phase of treatment is. Dealing with uncertainty is tough and coping well with it, ebbs and flows. That’s normal. I have talked about this in previous blog posts. I’m also nervous (my turn). I have a pet-ct scan coming up this week. Will the radioactive sugar stuff sent into my body find new lesions in my bone marrow, new weak spots or confirm that the treatment has worked brilliantly so far?
Maybe it is a good time to explore my relationship with illness and health. I can step out of project mode for a moment, round one of treatment has been accomplished. Now, is as good a time as any to face asking myself, in a more structured way, what it means to have incurable cancer, what it means to be ill. Which factors, which thoughts, beliefs, feelings and sensations are influencing my health behaviour, my coping…and not coping?
Psychology
One established psychological and behavioural model for explaining how we think about, respond to and manage threats to our health is Leventhal’s common sense model of self-regulation of health and illness1. Here are three of the concepts at the heart of the model.
- our perceptions of our illness directly influence our coping strategies, which in turn influence outcomes.
- our perceptions and resulting mental representations of illness and health threats have two parallel processes, a cognitive representation (our beliefs about; our identity, causes, consequences, timeline, coherent understanding and control/curability of our illness) and an emotional representation (our fear, distress, anger, worry, depression, guilt or other affective states). We use these mental representations to make sense of threats to our health.
- we actively engage in problem solving by testing coping strategies (aimed to manage fear from emotions, and danger from cognitions), and checking whether the coping strategies have worked, to help us reach goals (e.g. to overcome cancer, to survive as long as possible, to overcome anger and be the person we wish to present to the world/think ourselves to be despite illness or to be well enough to play with our children every day)
The model is one way of explaining how we go about reducing the tension that arises between holding on and letting go of important values and goals as we come under threat from ill health, disease processes and treatment impact and side effects. Figure1 below shows this in a bit more detail.
I thought I’d use this model to explore my thinking, beliefs, biases and assumptions about my current health. If you are managing pain, chronic illness, cancer or caring for someone who is ill, I hope you find it helpful to ask yourself similar questions. I encourage you to notice the thoughts that pop into your mind without judging them; they may surprise you. When I work with clients who are living with ill health using this model, they often discover something that they had no idea was influencing their sense of self, or making them feel worse or they discover a rule they had imposed on themselves, based on an unchallenged belief about what it means to be unwell or to be going to hospital or taking medication.
Where to start?
I start by asking myself;
what does ‘health’ and ‘being healthy’ mean to me?
what does being ‘ill’, ‘ill health’, ‘being sick’ mean to me?
Do these concepts mean different things when I think about myself versus when I think about others?
What does it mean to be diagnosed with cancer? With Myeloma? What does it mean about me that I have been diagnosed with cancer, with Myeloma? If it was my partner or a stranger with the diagnosis how would the meaning of having cancer/Myeloma be different?

Figure 1. Hagger and Orbell’s (2003) schematic representation of
Leventhal’s (1980) Common Sense Model of Illness (CSM).2
What do I ask next?
I explore a range of questions with myself about the mental representations I have about being unwell and under threat from cancer. While I work through each question and consider my answers, I also explore how my responses make me feel and what I will do to cope with the event and the feeling.
Stimuli
What am I experiencing?
What are my symptoms? (e.g. pain, fatigue, breathlessness)
What is telling me I’m unwell? (test results, pain, reduced mobility, hospital appointments)
What do I know about my illness?
Where is my information coming from? (external: medical team, support groups, google, other patients; and internal: physical and mental experiences)
What are my symptoms? (e.g. pain, fatigue, breathlessness)
What is telling me I’m unwell? (test results, pain, reduced mobility, hospital appointments, calls from medical team)
What do I think about where the information is coming from?
Cause
What do I think has caused my illness? Do I think any of it is my fault? Someone else’s fault? How has my illness come about? What do I think about the cause/s?
Consequences
What are the consequences for me, of my being diagnosed with cancer? From being unwell? What will I be able to do and not do? Will my life change? How will my life change? How will my relationships change?
What are the consequences for others of my being diagnosed with cancer? From being unwell? How will their life change?
Control /Curable
How much control do I have over what is happening to me? Over being sick? Over getting well?
How much do I think and believe my illness is; curable? able to be overcome? able to be managed well?
What do the consequences of the illness (e.g. likely outcomes, treatments, having to have chemo, a transplant, hospital visits and beyond) mean about who I am? what I am? My capabilities? My sense of being a woman? A daughter? A wife? A lover? An academic? A clinician? An exercise bunny? A coffee lover? Looking at all the aspects of my sense of self what does being ill, having cancer mean for each of those and who I am? No change? A change? For better? For worse?
Timeline
How long will I be ill? Will any changes and consequences be temporary? permanent? If my life changes will I be able to change it back once I am well or coping with the illness? Will it be the same as before?
Emotions
In addition to any coping strategies captured while gathering responses to the questions above…
How do I feel overall, right now, today?
How do I feel about being unwell? How do I feel about having cancer? How do I feel about each aspect above; the causes? The consequences? My sense of self? The controllability? Curability? How long I’ll be unwell? How do I feel about each of these? How do I feel about my thoughts and beliefs about each of these?
Coping strategies
In addition to any coping strategies captured while gathering responses to the questions above…
How will I cope? What am I trying? What makes me feel better? Feel worse?
What will I do? What will I avoid doing? Will I ask for help? From who and where will I ask for help? What will I practice thinking? Not thinking about? Where will I put my energy? What will I focus on? Avoid focussing on?
What emotions will I allow myself to express? Are there any that I am not happy to express? Why?
Appraisal of coping so far
What has worked well so far? What helped the coping strategy to work well? What hasn’t worked well? How did it not work well? What were the outcomes?
What do I want to change, try next, no longer try?
Working through these questions and using this type of model is challenging to do alone and isn’t something that is likely to be done and dusted in one sitting or even one day. It may take time to make the enquiry of yourself and find your answers. Notice the answers that pop into your thoughts, into your head. The answers may be scary sometimes, difficult to acknowledge or leave you feeling upset and distressed.
It is important to be kind to yourself during this enquiry. Its ok to take breaks. Its ok to feel distressed after noticing the answers. It’s a good idea to do something nice for yourself after working through these questions. These are difficult questions for anyone to look at, let alone anyone who is living with ill health or a life-threatening health concern.
Remember the aims of making the enquiry is to
- understand how we are making sense of our own health, ill health, diagnosis and health journey
- notice the factors influencing both our coping strategies and our appraisals of the outcomes from our chosen methods of coping.
- identify coping strategies that are likely to be most useful (complement our treatment and enhance our behaviour and management of illness, Myeloma) and drop the strategies that don’t work so well
Ultimately, by bringing our mental representations into our consciousness, our awareness, we may be able to pause and challenge some of them, more easily accept others, and create and foster new helpful health representations.
Many patients perceive they can stand extreme toxic Chemo therapy when they also hope and feel that it may result in a cure.3 There is no cure for Myeloma so how do Myeloma patients, how do I, stomach Chemotherapy? Do I stomach it because I hope it buys me time for living and time for a cure to be found, or buys me less pain, less discomfort, more quality of life? How am I managing fear control and danger control? What are my representations of illness? How vulnerable am I? How motivated am I to take self-protective steps? How easily accessible is my motivation? When is it easy, when is it difficult, for me to do the right things, to look after myself, adhere to medical advice, and adhere to the other complimentary advice I have chosen to follow?
Watch this space – I’ll post my answers over the next week or so to give you an idea of what this type of enquiry might look like…and then I’ll talk about what you might do with knowing your answers – how bringing the answers into your consciousness can help us to better manage the challenges that face us, illness based or otherwise.
Right now, I need a break so I only have one answer for you…
Beedie Beedie.
References
1 Leventhal, H., Meyer, D. and Nerenz, D. (1980). The common sense model of illness danger. In: Rachman, S. (Ed.), Medical psychology, Vol. 2. pp. 7–30. Pergamon, New York.
https://www.academia.edu/259452/The_Common_Sense_Representation_of_Illness_Danger
2 Hagger, M. S., & Orbell, S. (2003). A meta-analytic review of the common-sense model of illness representations. Psychology and health, 18(2), 141-184.
https://www.researchgate.net/publication/250571403_A_Meta-Analytic_Review_of_the_Common-Sense_Model_of_Illness_Representations
3 Cameron, L. D., & Leventhal, H. (Eds.). (2003). The self-regulation of health and illness behaviour. psychology press.
https://books.google.co.uk/books?hl=en&lr=&id=P3UoIuANmrIC&oi=fnd&pg=PR8&dq=The+self-regulation+of+health+and+illness+behaviour.+psychology+press.&ots=ARDdFKnVmY&sig=hU9R0fsNauKIs04RB3iezy-yAyA#v=onepage&q&f=false
Posted in Myeloma Treatment, Pain, Psychology for Cancer, Symptoms and Side Effects Tagged with: Apheresis, Cancer, Clinical Trial, Fatigue, Harvest, Myeloma, Para Protein, Psychology, Randomisation, Stem Cell Collection, Therapy, Transplant
July 19th, 2017 by Janine
I’m going to be sick. I’m running to the bathroom. I’m not going to make it. I’m scanning for basins and thinking use the kitchen if I can’t make it to the bathroom. At least make it to the tiles, it will be easier to clean up. I make it, this time. While I’m trying to keep my hair out of the toilet bowl and not notice how sore my knees are on the floor I start thinking; Where did this nausea come from? The last three months have been relatively easy; is this what Chemo is really like? Is this the nausea others talk about? Well they can have it back; it’s awful. And it’s not the worst thing.
I slowly make it back to the couch and lie down. I’m wondering if this last month of induction treatment is worse because I have responded so well to Chemotherapy over the last few months, now there is less cancer to vamoose; more good cells are copping it. I’m thinking about this when I notice my brain is getting hot. Not my head, not like a headache; my brain. In fact, its not just hot, it’s getting hotter by the second. My brain is on fire and I’m not sure I can cope. My eyes feel heavy…and hot. I can’t keep them open but I feel sick and am going to have to get up any second to go to the bathroom again. At this rate I’m going to need a couch near the bathroom or in it, not that it would fit. My brain hell fire is getting worse and my body is screaming at me to close my eyes, sleep, now!
I can’t, I have to go back to the bathroom. Ginger tea isn’t working this time. The anti-nausea pill isn’t working either. This chemo experience is different, and besides, I can’t keep anything down. So much for gaining weight or staying hydrated. A bit hard to do when I’m vomiting. I manage the journey to the bathroom, throw up and hang out for a while waiting for the next wave of nausea. I have a picture of my brain burning bright yellow and red with solar flare flames coming off the top of it, searing their way out of my skull. My brain feels like it is about to explode. It’s excruciating. Am I literally being fried with chemicals? I make it back to the couch and succumb gratefully to sleep.
From 4pm to 2am I’m in the bathroom or asleep. When I wake I feel trashed, tired but better. I eat two rice cakes and marmite (love it or hate it, it has its moments) and manage to take my meds. Relief. I feel slightly normal again. I watch TV for an hour and go upstairs to bed.
Sleep has been elusive over the last three to six months. I often wake every 1-2 hours. I am feeling a bit low and constantly tired despite the steroids. Unsurprising really when I’m not sleeping well. I talk to Dr L about pills and the nausea/brain fire. He takes control and agrees sleeping pills are a good idea and proposes a second anti-nausea drug. He doesn’t want me ‘putting up with’ anything. Relief again. I am finally going to get a good night’s sleep. Florence pops into my mind.
Music; Dog Days are Over, Florence and the Machine
For the first three months/rounds of Chemo I’d had no anti-nausea help and found using simple ginger tea worked. Now, I’m using two lots of anti nausea meds and ginger tea. The pfaffy thing; I need to remember to take the new meds 30-60 mins before food, three times a day. More stuff to think about when there are already so many pills and supplements to keep a handle on and information about upcoming treatment to process. Still, I’m highly motivated to prevent “brain on fire” and vomiting every five minutes – funny that.
The flag at Kings College Hospital is at half mast during my hospital visit, appropriately, for the victims of the horrendous attacks in London and Manchester. I feel strange too; grateful for not being in one of my favourite areas of London, an old stomping ground, at the time the attacker was there and yet also wondering how I would have reacted if it was me the person with a knife had come after. Does knowing you are dying sooner than expected change how you might react in crisis? Would I have run or taken more risks? Thrown things at the attackers, tried to fight back or help those that had been stabbed? Who knows? I can’t know. I’m grateful in many ways for not knowing and yet I’m curious about whether I would be different now.
The rest of month four passes without too many glitches and the best thing is getting some sleep – hurrah! I’m a bit depressed about how much strength I’ve lost though, and how old I feel when I can’t undo a jar lid or carry something I’d usually be able to carry. Weight training is now 20 reps of 1kg weights rather than three sets of 12 reps of a much higher weight. Fatigue is ever present.
This is not a novel new project anymore. The chemo, the eating regime, I’m over it. I want a break.
Editorial Support: Stephanie Kemp
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Myeloma Treatment, Symptoms and Side Effects Tagged with: Brain, Cancer, Fire, Myeloma, Nausea, Sick, Side effects
I bopped down the hospital corridor towards the Chemo Unit (listening to a bit of Adele) and started thinking back over this cycle of treatment. It’s not a good or bad news story. It’s a GREAT news story. Yes, there are a few side lines about niggly things, just to keep it real. Great news though; we can always do with a bit of that, can’t we?
Music – Music was back, yay! All a bit eclectic, and hey, that’s how I roll!
The theme-tune from Cheers: Where Everybody Knows Your Name, Gary Portnoy; On the Level, Mac DeMarco (calming and grating at same time); The Only Way Is Up, Yazz; Rapture, Blondie; An hour of Radio 1 in an afternoon; Right as Rain, Adele (transpose talk of lover with Myeloma; it works!)
Also gobbled up podcast S-Town, Serial Series 2 (Series 1 was great too).

Medical Update
Here’s a graph. I love a good graph, don’t you? I especially love this one as it shows some important stuff going in a mighty good direction. Cancer presence is trending down. My chemo response rate is trending up! Yeah, baby!!! I’m not fighting with Myeloma; I am guiding it to the door, hoping ultimately to close the door behind it for as long as possible.
The great news
My para-protein level, the indicator of those unwanted Myeloma plasma cells (now kicked to dust over the first two cycles of Chemo) is looking good, very good. My results have come down: from 40 g/l at diagnosis, up at 42 g/l when starting treatment, down to 17g/l by the early part of this cycle and by the third week, 11 g/l. The medical team look for (and the clinical trial requires for next step progression) a minimum of partial response (PR) by the end of the induction treatment (four cycles of Chemo). PR is a drop of 50% of presence of Myeloma indicated initially by the para protein level. The good news is that I had achieved PR by the end of Cycle Two! Also, the para protein level has kept heading in the right direction: down! I still have one cycle to go in this round so a great overall response rate seems so possible right now. And I am still gunning for 100%. I hope I am not too disappointed if 100% is not achieved.
The niggly things

It was a tough start to Cycle Three. I was feeling a bit low. On day one, Si and I attended a clinic appointment with my Clinical Trial lead. It was helpful, and he kicked off the conversation about the stem cell harvest. It was also awful. He went over the prognosis again: the incurable nature of Myeloma. Then he followed with the dramatic strides that have been made in the last two years with new drugs and better outcomes. They are better outcomes: people with Myeloma receiving treatment used to get three years, recently they were getting seven, and now the average is 8-10 years. Great strides, but still short, and I had trouble on that day hearing it all again. I wanted to focus on next steps in the treatment instead, not how long it may or may not ‘get’ me. I left feeling utterly drained and not overly well-informed about the cell collection as I had trouble listening to these points with loads of the other stuff in my mind creating noise.

While the scaredy needles seemed to get over their fear this month (Nurse L worked her magic), a strange rash appeared down my left arm (worse than the little bit I had experienced in early days of Chemo) and it hung about for a couple of days. No known cause at this stage and something to look out for again. My calcium level dropped a bit so I now take calcium tablets too. My urea and creatinine levels dropped for a week. These returned to normal after I focussed on keeping up the three litres of water a day and recognised night sweats might be dehydrating me a bit more than I had thought.
Long waits for Chemo occurred on a few days. One day was over three hours and down to a process issue; these kind of things happen sometimes yet are usually preventable. I gave what I hope was constructive and gentle feedback to the medical team. They were supportive, listened really well and agreed a plan of action. A Clinical Trial Nurse, M, thanked me for being an active partner in my treatment: for my feedback and follow up on things they have mentioned in the past, such as providing patient diaries and requesting new ones if they have not been received. Her comment felt genuine and I really appreciated it. I never want to overstep or cause additional work, yet my nose for process re-engineering and efficiency often rears its head, especially in the NHS. The NHS is awesome (free!) and could benefit from regular process review, especially as when used well, reviews and service/process development ultimately save time and cost. Hey, who has time to do timely reviews? More appropriate NHS resources required! Let’s hope Brexit doesn’t scupper that. Or the upcoming election.
Other great things; small and large
I attended a helpful webinar through MMRF that shared the latest USA understanding and treatments. Lots of promising diagnosis tools and new drugs are coming down the line that will hopefully be available in the UK by the time I need them, after my initial remission period lapses. I also attended a fabulous day at Kings College Hospital where the latest UK-based clinical trial information and outcomes were shared. We were given a tour of the labs in which blood and marrow are analysed, stored (at -196 degrees) and the clinical research facility. After donning the blue plastic shoes, hair bands and protectors to ensure we didn’t cause any contamination, we were taken into one part of the facility where we could safely view the highly-restricted areas and complex equipment – very ‘CSI’ (for anyone who has watched those TV programmes as much as I have). We learned about how contamination is monitored and prevented, and how studies of highly sensitive blood and organs are undertaken. Fascinating, and a real privilege to see ‘behind the scenes’ in this way.
My girlfriend B came along to Chemo with me on day 2 this month and it was so great to have her there. She was calm in a strange environment and we laughed together which was fab. Strangely, despite the circumstances, this day and another day on which we did meditation together and a third day when we made time for a great lunch date (unfortunately just before she left London; would have been great to fit in more of these) really stood out to me as special moments, quality time and very supportive.

We finally christened the table tennis table (Si’s birthday present). I am queen of the table; the presiding champion in the round robin between Si, my brother-in-law and me. Of course, were you ever in any doubt? Si didn’t like that and brought up other stories about me beating him at clay-pigeon shooting over ten years ago during another birthday present experience for him. Ooops! Although, wait until Mum gets here, she tends to claim table tennis crowns!

On the last day of Chemo this month, I wore a dress and two people told me I looked lovely. What a great start to the day. Especially as I felt very tired that morning. Choices again. I could have worn tracky bottoms and a top like I did the day before and that would have been fine. I needed a pick-me-up. A dress and makeup was a helpful move. After all, I felt better. It was great to dance in on the way up to Hospital, feeling the fabric move around my bod. And hey, it resulted in compliments – the dress, not the dancing! Worth it, that little bit of effort. I might not have the energy to do this next time and that’s ok. It was lovely to grab the moment on that day.
Thank you
Thank you to you, the readers; there are now over 800 users on the Psyching Out Cancer blog.
Psychology – Reflection
Life is a daily, weekly, yearly roller-coaster of good, difficult and neutral events that come and go. Our response to each event – small or huge, the attention we give each, the meaning we add, the willingness to accept the unchangeable – all dictate how we well we cope with the rollercoaster. Our ability to pause, notice, and choose a response, facilitates how much we stop and enjoy the good times, and ensures the more difficult times have less impact on our day to day lives and long term goals. Sometimes though, we forget to pause or find it difficult to pause; this is where in addition to knowing our triggers for unpleasant reactions, Reflection is crucial.
Reflection is defined as serious thought or consideration. In psychology, reflection often involves a therapist reading or saying the client’s words back to the client so that they can hear for themselves what they have said and evaluate the logic or reasoning behind their own statements. You can also be your own therapist with reflection. Self-reflection can be referred to as examination and contemplation of our own thoughts and behaviour; helping ourselves to hear and evaluate.1-3
There can be no knowledge without emotion. We may be aware of a truth, yet until we have felt its force, it is not ours. To the cognition of the brain must be added the experience of the soul.
Arnold Bennett (1867–1931) 4
The lessons I have learned, and psychology skills I have applied, this month have often been difficult to remember to use in a timely manner and I have needed time to notice and understand my reaction and needs. The post reflection lessons have been transformative and confronting; they have led to open, honest debate with myself and communication with others such as in my previous post ‘Killing Me with Kindness’.
All in the Mind, a BBC Radio show presented by Claudia Hammond, is a fabulous resource for learning about mental health (links below). The show often hears from people with experience of mental health difficulties, charities working in this space, expert clinicians, and academics and researchers who explain the latest evidence about incidence and treatment, and debunk myths. In one of the recent episodes, evidence was presented about the power of expressive writing about your experiences and the positive outcomes that were experienced.
Writing can be, for some, a great way to facilitate reflection. Whether it is keeping a diary, or writing a letter to yourself or another, writing about how events made you feel emotionally and physically, the thoughts you noticed, what you were curious about or wondered about in terms of the event, yourself, the other person’s thinking, feelings, reaction, motivations. It can be so helpful to ‘not to make the person wrong’. Instead, focus on the event or behaviour and how it made you feel, how you thought it might have made the other person feel, with curiosity and compassion. Recognise that you may have their feelings and thoughts wrong; be careful not to assume and instead be curious. You do NOT have to send the letter. You do NOT have to keep the letter once it is written, though you may find it helpful to send or re-read them; only you can decide this.
For those that don’t like writing, a Dictaphone, a voice recorder, or even an app that converts your voice to word or pages can be used.
If neither of these appeals, taking time out simply to be and think about a past event, day, week, a particular period, can be useful. Notice all those things above, and also notice what worked well, what worked less well, and what you would do differently or not do differently.
Alternatively, and I highly recommend this approach (which can be done alone or in combination with the others above) solely focus on taking time to sit, put yourself back into the event and be with whichever emotions, light or strong, arise. Allow yourself to feel them, deeply, outwardly with tears, or anger or another response, if that is what arises, without judgement of yourself or anyone else. This type of reflection helps your body and mind to fully experience and process events together. Regular reflection, not rumination where negative thoughts are given repeated attention, but regular curiosity-based reflection, can help process strong emotions.
All regular reflection can help your mind and body notice when similar events are happening again, often earlier than usual, and sometimes even in the moment. This observation then allows for pause and choice of response; helpful or unhelpful, one that serves you well or doesn’t serve you well.
Remember, after reflection, be kind to yourself; your responses and emotions within reflection are normal. If you feel upset or angry afterwards, take 5 minutes or more to do something enjoyable even for a few minutes; take a few deep slow breaths; tell yourself you are ok, safe, good enough; read a magazine; do one yoga sun salutation; make a cup of coffee; close your eyes; do a body relaxation exercise, a tai chi movement, a back stretch or something else relaxing and fun to bring your arousal level down before trying to get on with your day.
Summary
Reflection is an important skill for maintaining good mental health and one worth investing time in practicing: through writing, dictating or focussing on your experience in a curious way that allows you to fully experience your emotions.
Great News
Cycle Three – done. A roller-coaster and many highlights of great news. Onwards with Cycle Four, the last month of Chemo before the next phase of treatment. Gosh, the time has gone quickly.
Resources
BBC – All in the Mind. http://www.bbc.co.uk/programmes/b006qxx9
All In The Mind, Episode including benefits of expressive writing (15 May 17) http://www.bbc.co.uk/programmes/b08n2wcz
Gibbs Reflective Cycle (in Dye, 2011), University of Cumbria (2016)
http://my.cumbria.ac.uk/Public/LISS/Documents/skillsatcumbria/ReflectiveCycleGibbs.pdf
Acknowledgements
1 Oxford Dictionaries https://en.oxforddictionaries.com/definition/reflection
2 Alley Dog Psychology Glossary https://www.alleydog.com/glossary/definition.php?term=Reflection
3 Psychology Dictionary http://psychologydictionary.org/self-reflection/
4 A return to the use of emotion and reflection. Helen Demetriou and Elaine Wilson
https://thepsychologist.bps.org.uk/volume-21/edition-11/return-use-emotion-and-reflection
Images: B, Me
Editorial Support: Stephanie Kemp
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Myeloma Treatment Tagged with: Cancer, Myeloma, Para Protein, Partial Response, Psychology, Reflection, Response Rate, Survival Rates

Causes, Choices, Control and Change.
Now that I have circumnavigated the first two months of treatment, with a focus on doing what had to be done, I notice the question of ‘Why Me?’ popping into my head more often. I think about causes, choices, control, and change. What caused my Myeloma? Why Myeloma and not another cancer? Did my past choices cause my Cancer? What can I control now? How do I keep control? What should I change about myself? What should I change about my lifestyle? If I make changes, will my prognosis be the same? Will changes really make a difference? Or will I just think changes make a difference? Will I create false hope? If I make a bunch of changes and my cancer gets worse, or remission is short or only the same as every other person with Myeloma, will I feel cheated, get depressed, wish I’d just carried on as normal and not changed anything? Are thinking about causes, control, changes and choices like a mouse going down a tunnel with no cheese? Which are illusions, which are realities?
Ultimately, the question I was asking myself was: “Should I change my terrain?”
The main areas of terrain I was considering were:
- Nutrition
- Chemicals/Toxins
- Mobile Phone / Technology
- Mindfulness and Meditation
Why the focus on these areas of terrain?
I was considering these areas as they made sense to me as possible areas for change. The science, while not based on randomised control trials, is compelling and pointed out in an easy-to-read book called Anti-Cancer, a new way of life by Dr David Servan-Schreiber (who also had cancer).
After all, it is unlikely that there will ever be large swathes of money on offer for randomised control trials (RCTs) about Nutrition for Cancer when Big Pharmaceutical companies are competing for the same pot of money for their new drug… or when the findings from Nutrition trials may potentially show there is no longer a need for an existing drug that makes someone a whole lot of profit right now.
Don’t get me wrong, I am very grateful for Big Pharma, their RCTs and their drugs; they are helping me to kick Myeloma into remission. I am however, a strong advocate for a holistic approach; an informed meld between medical and non-medical models, especially as the West learns to give more open consideration to healing and health strategies that have been used by non-Western cultures for centuries.
Particularly too, as while Cancer effects people of all ages and socio-economic status, it appears to predominantly be…drum roll… a first world country problem. Why is it that the rates of Cancer are very high in some countries (France, Denmark, USA, New Zealand and UK) in comparison to other countries (Japan, India, Oman). Why is it that more developed countries fair worse than less developed? 268 cases of cancer were diagnosed per 100,000 in more developed regions, compared to 148 in less developed regions in 2012, with an exception being the non-melanoma skin cancer rates which were higher for less developed countries. Why do other countries have crazily high rates of people with major illnesses other than cancer, such as heart disease (Turkey, Russia)?
Although diagnosis and recording systems availability and accuracy may influence data, could it be that certain types of stress, food, individualistic societies or combinations of these are also having an impact on cancer rates?
‘Why Me?’
I indulged my ‘Why Me?’ for a short time and asked: “Was it because I had chronic stress for years?” Was it because, before changing career, I had worked in contracts for telcos and banks, with constant tight deadlines, crazy commutes (5 hours a day at one stage) and a feeling of always having too much work and never getting it done? I wondered, did I get cancer because I’d lived on coffee for years, eaten too much chocolate, cake, biscuits, drunk too much alcohol during my twenties (and thirties)? Or was it because I was too analytical, too ‘in my head’, ‘too something’? Was this my path, my destiny? Was I meant to learn something? Be something from this experience? Did I even believe in paths, fate, non-fate?….and so like any normal human ‘bean’, I dwelt for a little while and still do occasionally. And, this IS a tunnel with no cheese. This conversation with myself, doesn’t serve me. I don’t hang out there for long.
A reality.
We (me, my medical team, the fatalists and non-fatalists in my life) don’t really know the answer to Why Me? When I asked the medical team, if anything I had done, used or consumed, caused the Myeloma, they insisted there is no evidence for links between my list and people getting Myeloma. I rattled off: stressful jobs; caffeine and alcohol; supplements; skin potions and lotions; whacky, at the time, spa treatments; and, multiple surgeries (involving though not exclusively, three knee and a number of IVF related invasions).
It may be something I’ve done or something I haven’t done, something about my biological make up, my vulnerabilities, the years of chronic stress, the coffee or lack of coffee (I went without for a year) or some very specific combination of some, or all of these, in very specific amounts of severity, for a specific duration. Are you noticing the complexity of ‘cause’ here? No one really knows and no one may ever know. There may be some amazing medical breakthrough in two years, 4 months and 6 days, when someone is studying finger surgery and discovers something new about Myeloma, that then leads to a randomised control trial or DNA discovery that may indicate some possible cause of Myeloma.
Let’s face it – right now, what we know is, Myeloma strikes at random and in general, men over 70 years old seem to get struck a little more than most. Until such time, as some crazy discovery is discovered, there isn’t much point me thinking about ‘Why Me’?
Yet…..
I can’t help thinking, if I don’t change something about: how I was living, what I was putting into my body and, how I was thinking, I’ll invite the status quo or a repeat performance. That is, won’t I be inviting Myeloma to return once it is in remission, if I don’t change the terrain in which it developed, ran amok and was diagnosed? This is the possible illusion as today’s reality (medical knowledge) indicates Myeloma always ultimately returns and people living with Myeloma eventually stop responding to treatment (drugs and transplants). However, making changes and choices, help a person to feel in control of their day to day or to feel they have some control over their illness: another illusion? Possibly…but….
What if changing my terrain works?
If I changed my terrain and it didn’t change my prognosis or my response to treatment, I would be disappointed but at least I’d know, I had done the best I could. No regrets. Or would I think, sh*t I should have just had chocolate fudge cake whenever I felt like it, three coffees a day (and thrown in margaritas and champagne regularly) because it probably didn’t make a blind bit of difference?!
Regret?
But what if it did work? What if I changed my terrain: changed my nutrition; removed my mobile phone from the bedroom; replaced my cleaning products with eco friendly, less toxic ones; used only ‘safe plastic’ or glass to store food; changed my skin care products to chemical free, natural ones; and practiced mindfulness and meditated regularly? What if, after all of these changes my response rate to Chemotherapy was excellent and my remission period was longer than average. Wouldn’t the choices, changes and exerted control be worth it?! SO, what choice do I have, really? How will I know what difference change makes, without making change? If I don’t make all the changes, all at once, don’t I risk missing out on gaining the full benefit, if there is a benefit to be gained?
Causes, Choices, Control and Change – both illusions and realities.
I don’t know the cause of Myeloma. I don’t know if my past choices had any influence over whether I got Myeloma or not. I don’t know if my present and future choices will influence how my Myeloma treatment, prognosis and experience will play out. The only thing I do know, is that I can choose to change and making changes may help me to feel in control. Taking control and making changes may have a positive impact on my lifetime outcome and my experience of the cancer journey or at the very least it may help me to feel some semblance of lack of regret.
Psychology – Choices.
What I also know (though it can be easy to forget this) is that I can always choose to review my choices regularly and change them. No one is stuck with a choice. It might feel like it yet we make dozens of choices every minute of the day – which direction in which to move, what to say, to eat or not eat if we have food, where to look. We can keep choosing even about the big-ticket items in our life. Just because we take one path doesn’t mean we can’t, pause, reflect, review and make another choice or reaffirm the choice we have made.
For example, each day for the last six weeks, I chose not to have coffee. Now, I’m going to get one, and savour it. You might say, well if you were a smoker trying to quit smoking, a choice of having one cigarette may be a poor choice. I might choose to agree. Alternatively, I might choose another tack and say that the smoker trying to give up who finds his/herself having one cigarette, could choose to not ‘beat their-self up over it’; they could choose to recommit to their goal of giving up and choose in each minute, to not have a cigarette. Better yet, they could also choose to make a positive healthy, non-cigarette involving choice, about what to do and where to place their attention. In other words, I would encourage positive choices that serve them and their goals.
Now relate this to Chemo and Changing My Terrain. Two months ago, I chose to start Chemo. Tomorrow, I might choose to stop. I could. I might. Right now, I have reviewed my choice and I am happy with my choice to do Chemo and be in a clinical trial. It doesn’t mean I can’t choose differently tomorrow, if I so wish. Let’s take a breather now; more about choices and attention later. Hmmmm, smell that coffee.

Acknowledgements:
World Cancer Research Fund International
http://www.wcrf.org/int/cancer-facts-figures/data-cancer-frequency-country
http://www.wcrf.org/int/cancer-facts-figures/comparing-more-less-developed-countries
World Health Organisation
http://www.who.int/nmh/countries/en/
Editorial help (any errors are solely my own): Simon Hayward and Belinda Marment
Illustration: Sapphire Weerakone
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Myeloma Treatment, Nutrition for Cancer, Psychology for Cancer Tagged with: Cancer, Cause, Change, Choice, Control, Lifestyle, Mobile, Myeloma, Nutrition, Terrain, Treatment, Why Me
It’s been hard to write the blog in week’s four, five and six of Chemo; I didn’t know where to start, there didn’t seem to be time, and I was worrying. Even Music didn’t show up much; I didn’t hear it or go looking for it – strange.

I started to worry about having little time; not time on this earth but time during the day to do all the things I needed to do. Sound familiar? I have learned over the years that when I worry about not having enough time, it usually means I am probably trying to do too much and am not getting enough rest or chill space. I noticed too that when reminders popped up in my calendar to get some ‘headspace’ or do a visualisation, I was swiping them away and thinking I’ll do that later yet later never came. This worried me.
I wondered whether my blood test results for week four would not be as good as the previous weeks and imply that going away to Canada had been a bad call after all. It turned out this worry, while natural, was unfounded; my results showed more test results falling within the normal range than in the previous weeks and suggested my immune system was hanging in there – a good result.
I worried about an interaction with a Nurse and found myself feeling ‘told off’, then wondering if I was being over sensitive, or not sensitive enough to others. I felt guilty for coping well with and doing well on Chemo. The nurse had asked how I was doing and I had said something along the lines of “really well thanks” and “chemo had been quick today”. I heard a response of “well that’s not the case for everyone”.
Then a stream of thoughts flooded my mind;
- Sh*t, had I spoken too loudly?
- A lot of people look very ill and drained on the Chemo ward today, have I not thought of them? Should I think of them?
- I have answered honestly and positively; that’s what I committed to do throughout this process wherever possible.
Feeling a bit indignant, more thoughts rushed in;
- No, it’s fine for me to be positive after all it’s not my fault I’m doing well,
- Being positive is meant to help with healing so I’m not going to stop answering ‘I’m Doing Well’, when I am doing well.
Overnight and with reflection I decided I probably was being a bit sensitive and it was also fine to be positive. The following day I checked in with the nurse, who quickly reassured me that he had not thought I’d been insensitive to others on the ward at all. We cleared any misunderstanding and he reiterated how great it was that I was doing well. This frank discussion helped bring clarity and perspective to my thoughts. It stopped this worry completely. I’m glad I raised it with the nurse even though I was uncertain (and nervous) about what I might hear.

Despite this resolution, a residual sense of stress, worry and an over active adrenal system remained; the opposite of the many calm moments that I had been experiencing last month. The overall worrying continued.
My weight had dropped again to 66kg and I was struggling to eat enough calories. I often didn’t feel hungry but still tried to eat. I hoped my weight would stabilise and even climb back up to 68kg. That weight had felt comfortable while now I noticed I didn’t seem to have much padding, wondered if I really did have much of a reserve if I got an infection and I noticed I had lost muscle mass. The backs of my hands look like some very elderly person’s hands; dry and wrinkly despite the constant fluid intake. I worried that my weight would keep falling and my skin would get worse.
I worried about whether I should stick to the plan of not working for six months to focus on getting to remission as successfully as possible or to work while I still could. I worried about if I worked, would it be too stressful, leave me enough time to rest or feel like it’s getting in the way. I worried about not being able to work out how much work was too much, and for private practice whether enough work matched with breaking even financially. I worried about how to contain my clients’ concerns if my appearance changed with more chemo and how I provide a consistency of safe space for them if my medical appointments needed to change in the future. I worried and yet I missed making a difference and being the psychologist I know I can be.
To cap off the week, I finally had a long-awaited Ear, Nose and Throat appointment (yet another hospital visit) to check my possible hearing loss. This is something else I have been worried about for a long time and that has no doubt been bugging Si for years as I constantly ask him to repeat himself or need the TV volume well above the level he would choose. I had noticed my hearing was worse when; I’d find it difficult in crowded places (and with background noise) to hear the person I was standing next to and speaking with, or to hear what someone was saying if I couldn’t see their face and mouth. I noticed I had started guessing (not always accurately) what someone was saying.
For a psychologist; listening skills are imperative and before listening skills can be invoked one has to be able to hear! While I had rarely experienced these problems in one to one therapy sessions, I was concerned symptoms would get worse or impact my functioning. Sure enough I wasn’t dreaming this either; tests showed my hearing has deteriorated though is still in the mild loss range; inner ear cochlear deterioration so unrecoverable. This is essentially the kind of loss most people start experiencing from around 60 years old on…except I’m not 50 yet! I suspect I’m paying the price for good times; a burst ear drum while scuba diving as a teenager and damage from standing far too close to speakers at Fabric nightclub a few years back (ok, so quite a few years ago now).
So I’ve been worrying and it’s completely natural to worry. It is not helpful to dwell in worry or worry about things I can’t control so how do I let go of it? Worry is something I have helped many clients with over the last ten years so it is definitely time for some self-help. Below are the psychology tips and strategies I reminded myself to use.
Psychology – Overcoming and managing worry

What is Worry? How worry works.
Worry is a form of mental problem solving about potentially negative future events. It can be triggered by a variety of external events or from thoughts that just pop into your head. Worry is characterised by a lot of ‘what if’ questions. For example, ‘What if my Chemo doesn’t work?’ ‘What if my new boss doesn’t like me or think I’m good enough?’
Normal worry is usually short lived and leads to positive problem solving activities. Worry becomes unhelpful when it is about several things, is frequent and difficult to control or dismiss. We can think prolonged or frequent worry helps with problem solving, planning and preparation however worry breeds more worry (and anxiety) which prevents positive thinking and action.
Worrying can rob people of time. It’s exhausting and often leaves people feeling tense, with disturbed sleep, difficulties concentrating, and feeling irritable. While sometimes it can feel appropriate or necessary, worrying is exactly the opposite; it’s restrictive, and takes up time, attention and energy that could be spent on useful, enjoyable and meaningful activities.
Why do some people seem to worry more than others?
Worrying is human! The causes of are not clearly understood though it may be that a number of vulnerabilities increase the chance of developing a tendency to worry excessively; prolonged stress, past experiences of uncontrollable or traumatic events, an inherited biological disposition to experience negative emotions, learned messages from others that the world is unsafe or that worry is useful, and a coping style that involves avoiding challenges or situations where there is a chance of experiencing negative emotions (which prevents positive experience of coping and positive emotions).
Managing worry.
UNDERSTAND YOUR WORRY CYCLES – Understand your vicious cycles of anxiety and how avoidance contributes to anxiety. See the handout below (CCI – Vicious Cycle of Anxiety).
NOTICE YOUR PAYOFFS AND COSTS. Part of understanding your worry can be to notice if you are getting a pay-off from worrying, ‘buying into it’ and most importantly what the cost of the pay-off might be. Are you avoiding going out? You might get a pay-off of avoiding any negative emotions such as uncertainty of what will happen or be said when you see someone but you also miss out on the potential positive experiences; fun, laughter, connectedness or ease which going out may also provide. Also notice, where do you worry and what are you doing when you worry. For example, are you sitting down and telling yourself ‘you are worrying but getting rest at the same time’. Consider that your type of ‘sitting down’ in this instance is not truly restful and what it actually costs you is feeling rested. If you shifted your attention away from worry to giving yourself permission for genuine rest, and allowed yourself to do something enjoyable without the worrying in that same time, you are much more likely to feel rested and relaxed (and be better able to cope with normal levels of worry that we all experience).
Other practical strategies:
USE A WORRY TREE to identify where to put your attention so that you shift your attention to worries you can do something about and form a plan for rather than worries you have no control over. There is a link to a handout below
CHANGE “WHAT IF’ STATEMENTS TO ‘HOW’ STATEMENTS’. For example, instead of “what if Chemo doesn’t work?’ I might ask myself ‘How will I act if Chemo doesn’t work? How will I find out what action can be taken next?’
POSTPONE WORRY. This is where you give yourself permission to worry about a specific topic, at a particularly time later in the day, for a maximum duration of say 20 minutes). This way you are acknowledging your concern and allowing yourself to think about it for a contained amount of time without it taking over and impacting the rest of your day. Sometimes you may find the thing you were worrying about has resolved itself by the time the allotted worrying time has come around, or it looks completely different and isn’t as big of an issue as it seemed earlier or doesn’t have to be dealt with today after all.
Summary
These are just some tips for managing worry and there are others if these don’t work for you. Remember, while worry is normal, excessive worry can be gripping and creep up on anyone. Even when worry can feel like a good thing to do, it creates more anxiety. When it stops you from enjoying life or doing the things you want to do, worry is not your friend. Excessive worry can be overcome. Please try the strategies outlined above and the links to helpful handouts below. If you find them hard to do alone, do talk with your GP or ask a psychologist to help with gaining treatment or to work through the strategies with you.
Acknowledgements, Permissions and Helpful Handouts:
Centre for Clinical Interventions (CCI), Department of Health, Australia http://www.cci.health.wa.gov.au/
CCI Generalised Anxiety and Worry
http://www.cci.health.wa.gov.au/resources/infopax_doc.cfm?Mini_ID=46
CCI Vicious Cycle of Anxiety
http://www.cci.health.wa.gov.au/resources/docs/Info-Vicious%20Cycle%20of%20Anxiety.pdf
CCI Postponing Worry
http://www.cci.health.wa.gov.au/docs/ACF3D66.pdf
Get Self Help Get.gg – Worry Tree
https://www.getselfhelp.co.uk/docs/worrytree.pdf
Images: Simon Hayward
© 2017 Janine Hayward www.psychingoutcancer.com. All rights reserved.
Posted in Chemotherapy for Myeloma, Psychology for Cancer Tagged with: Cancer, Chemotherapy, Myeloma, Psychology, Worry
April 24th, 2017 by Janine
Aside from the Chemo, my body has consumed at least 534 medications and 825 supplements in the last 50 days….1359 pills in all.
I visited a well know artist with a gallery in South London. I tried to have an open mind but still came away not liking the art!
I did discover the gallery has an interesting cafe based on a pharmacy (and one of the artist’s famous pieces) with an array of pills show cased all over the walls. If I post pics of all of my pills do you think he’ll come after me for plagiarism?!
My average day….

I’m officially a pill popper!
Posted in Myeloma Treatment, Nutrition for Cancer Tagged with: Cancer, Medication, Myeloma, Pills, Supplements, Treatment, Vitamins